I’m pretty sure you’ve heard of Polycystic Ovarian Syndrome (PCOS)—it seems to be everywhere these days. In fact, it happens to be the leading cause of infertility in the United States and is estimated to affect 20% of women in their childbearing years! Despite its prevalence though, there still remains an ongoing debate regarding its cause, and why it appears to have become an epidemic in so many western countries.
Unfortunately, the medical industry has put its focus on treating the symptoms of this condition through medication, like the birth control pill and metformin, rather than addressing the root cause. This has led to the widespread misconception that PCOS is an unpreventable and incurable disease. I’d like to dispel the myths that have led many women diagnosed with this condition to feel helpless in their abilities to take control of their own recovery and hopeless in their dreams of one day having children. PCOS is not only treatable, it is preventable, and even (dare I say it) curable.
What is PCOS?
PCOS is a condition characterized by excess androgens (male sex hormones like testosterone) that causes symptoms like irregular menstrual cycles, head hair loss, body hair growth (especially on the face), mild to severe acne and even depression. But to get to the heart of what’s happening in our bodies that leads to PCOS, we need to start with insulin.
Insulin (the blood sugar hormone) is released into our bodies in response to sugar in the bloodstream. Its purpose is to grab this sugar from our blood and get it into our cells so that it can be burned for energy or stored as fat. Healthy complex carbohydrates break down gradually in our bodies, keeping our insulin and sugar levels balanced with only slight increases after meals. But when we eat unhealthy refined or simple sugars (think cake and cookies, white bread, white rice) these break down much more quickly causing a dramatic spike in our insulin levels.
Remember, the purpose of insulin is to escort sugar from our blood to our cells, so this huge spike that occurs when we eat  refined sugars causes more sugar to get pulled out of the blood a lot faster than normal. This in turn causes a drop in our blood sugar levels which then leads us to crave more sugar to bring our blood sugar levels back up. And around and around we go. I like to call this the Blood Sugar Roller Coaster. Not as much fun as it looks!
refined sugars causes more sugar to get pulled out of the blood a lot faster than normal. This in turn causes a drop in our blood sugar levels which then leads us to crave more sugar to bring our blood sugar levels back up. And around and around we go. I like to call this the Blood Sugar Roller Coaster. Not as much fun as it looks!
Why is insulin harmful in large amounts?
Eventually, if we continue with this vicious cycle, our bodies will build up a resistance to insulin. What this basically means is that the insulin in our system is no longer doing what it used to do (escorting sugar out of the bloodstream to our cells). But our bodies don’t know this, so the pancreas continues to release more insulin into our blood to bring down the sugar levels, which eventually leads to high levels of both glucose and insulin in our blood. What does all of this have to do with PCOS, you might be asking? Well, here’s your answer…
Actually, there are a number of answers:
- Most women who have insulin resistance also have high androgens (a fancy word for male sex hormones). The reason for this is that high insulin causes the ovaries to make excess androgens, in particular testosterone.
- In addition to that, excess insulin causes the liver to make less sex hormone-binding globulin (SHBG), the main protein that binds testosterone and keeps it from running amok. This creates more free testosterone and the potential for PCOS symptoms.
- Insulin resistance raises aromatase activity, the enzyme in charge of making estrogen. This can create estrogen dominance and reduce regular ovulation.
- As if this wasn’t bad enough, insulin is also a fat storage hormone, so
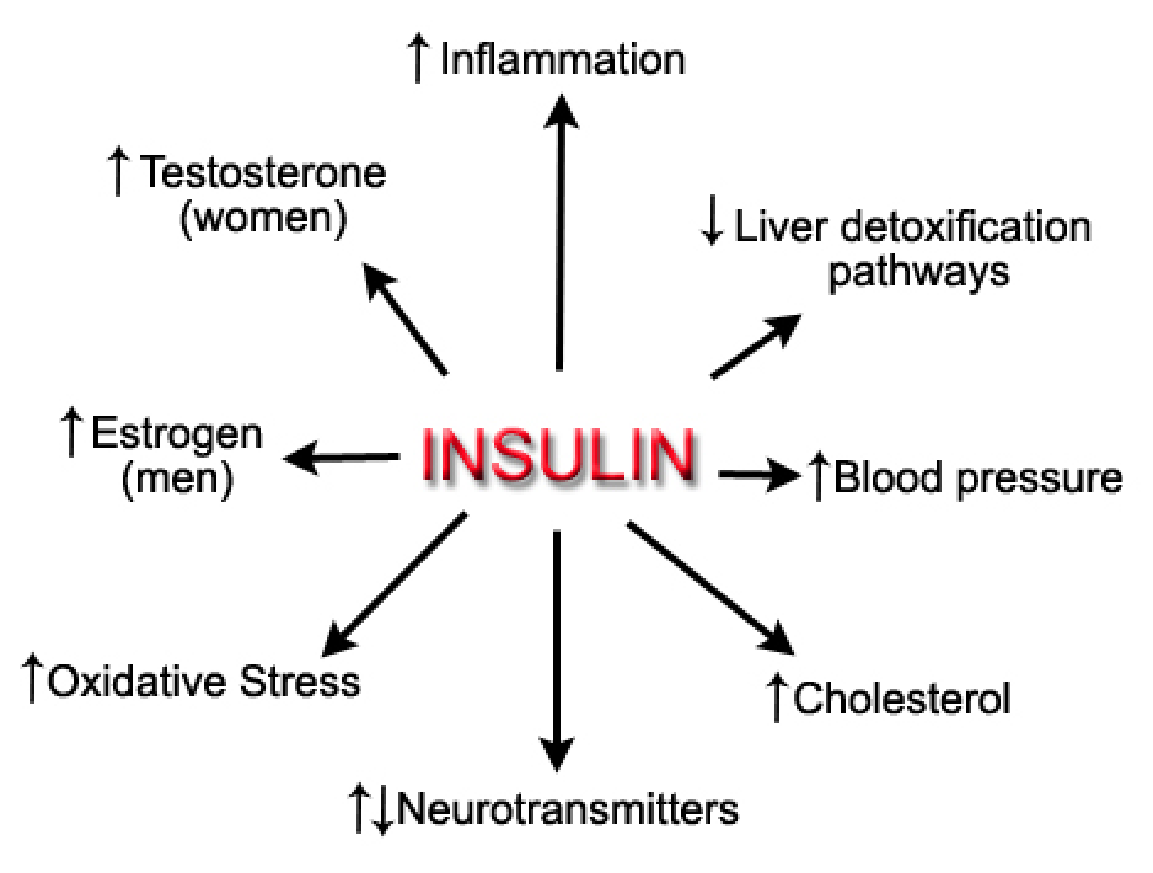 you will also start to put on weight, especially around your waist, and have difficulty losing it too. Muffin-top city!
you will also start to put on weight, especially around your waist, and have difficulty losing it too. Muffin-top city! - Unfortunately, this excess body fat causes many women to produce even more testosterone and estrogen which can block the pituitary gland from making adequate follicle-stimulating hormone (FSH). This leads to an imbalance of luteinizing hormone (LH) in proportion to FSH. FYI: FSH stimulates the follicles in our ovaries to grow and LH is the catalyst for ovulation. Too little FSH means that the follicles in your ovary cannot mature adequately which means the dominant egg is never formed. Instead, all that is produced is many immature follicles, which end up becoming cysts on the ovaries. And that is what we have come to call Polycystic Ovarian Syndrome.
For a slightly more in-depth look into how insulin affects our hormones, check out my previous post on PCOS!
Is being overweight a cause of PCOS?
When a patient is diagnosed with PCOS, a handful of doctors will automatically jump to weight loss as a treatment option. While this may be necessary for some, it does not get to the heart of the problem. In fact, weight gain is always the symptom of a much bigger imbalance in the body—and it’s usually this imbalance that is causing the PCOS as well. That said, to simply state that patients should lose weight without informing them as to why or how, implies that weight loss—by any means—will be beneficial for treating their PCOS symptoms. This can be a dangerous implication. Many women, for example, will take aggressive and extreme approaches to shed pounds, increasing their stress and cortisol levels in the process, and further throwing their hormones out of whack.
It’s important to mention that weight gain can also be a symptom of PCOS! A recent study shows that almost half of PCOS sufferers also suffer from hypothyroidism, a condition in which the thyroid is unable to produce sufficient amounts of thyroxine (T4) and triiodothyronine (T3)—two hormones instrumental in the body’s metabolism. Women who suffer from this will find it very difficult to lose weight, especially with stressful restrictive diets and hardcore workout regimens. As with PCOS, hypothyroidism needs to be treated at the roots, not the symptoms: the objective should not be losing weight, but rather regulating the patient’s hormones through gentle dietary and lifestyle changes in order to get her body back to working the way it was designed to work. (Losing weight will often be a byproduct of the healing process.)
Now that we’re all caught up there, let’s get into specific tips to treating your PCOS naturally!
What are the natural treatment options for PCOS?
So now that we’ve got a picture of what is happening in our bodies that leads to PCOS, let’s talk about the natural treatment options that are available for those who have been diagnosed with this condition. As you know, I’m ALL about empowering women to take back control of their own health, especially their menstrual health, so here are some really practical steps to take right now to address PCOS naturally:
- Low-glycemic love – The goal with runaway insulin is to rein it back in so that you can lower
 excess androgens. The best way to do this is to start incorporating low-glycemic food immediately. On a scale of 1-100, any food below 55 is considered A-OK in my book. Here’s an example: a bowl of cornflakes has a glycemic index of 93 while an apple is 39. Any carbohydrate-heavy food is gonna be a no-no. Sorry, ladies. 🙁
excess androgens. The best way to do this is to start incorporating low-glycemic food immediately. On a scale of 1-100, any food below 55 is considered A-OK in my book. Here’s an example: a bowl of cornflakes has a glycemic index of 93 while an apple is 39. Any carbohydrate-heavy food is gonna be a no-no. Sorry, ladies. 🙁 - Sugar baby – The low glycemic paragraph above would not be complete without a small lecture on sugar! I know it’s irresistible to many of us but as you know, it increases glucose and insulin levels which as you now know, increase those boy hormones. No good. Try curbing cravings with coconut butter, a yummy, low sugar treat—truly divinity in a jar!
- Fabulous fiber – Did you know that fiber increases elimination of testosterone through the bowel? Hail mighty fiber! If you have PCOS, and even if you don’t, you should be getting 35-50 grams of fiber a day. This is because without sufficient fiber, testosterone can be reabsorbed
 and used all over again! Eeeks! So work on getting those beans into your diet—a cup contains anywhere from 10-20 grams of fiber depending on the type of bean.
and used all over again! Eeeks! So work on getting those beans into your diet—a cup contains anywhere from 10-20 grams of fiber depending on the type of bean. - Omega-3’s please – An interesting fact: women with more omega-3’s in their blood have lower androgens. All you have to do is start incorporating more wild Alaskan salmon and a high quality fish oil supplement that is free of impurities. Rosita Extra-Virgin Cod Liver Oil is the supplement I use and recommend. Make sure to get at least 2000 mg of fish oil a day if you supplement.
- Vitamin D – If you have PCOS then you are very likely to be lacking vitamin D—44% of women with PCOS are lacking in the sunshine vitamin. Go out in the sunshine between 10am-2pm without sunblock every day to start building up your vitamin D levels. I also recommend supplementing with Seeking Health Vitamin D3 + K2 capsules.
- Chromium – Chromium is a mineral that promotes proper insulin utilization and helps with blood-glucose management. Hello, chromium! Goodbye metform! Just kidding, but not really… 🙂 The USDA says that 50% of Americans are deficient in chromium so clearly there is a correlation to the high incidence of insulin resistance, diabetes and PCOS. Chromium can be found in a wide range of foods, including broccoli, sweet potatoes, grass-fed beef, raw onions, and eggs. You can also supplement with 500 mcg of chromium picolinate a day to address your blood sugar issues.
- Magnesium – Most of us are deficient in magnesium, which is crucial for blood sugar balance, stress management, and sleep! Aim for 350 mg of magnesium every day, in the week leading up to your period and during your period. Or better yet, try for everyday of your cycle. It takes just 2 cups of spinach or swiss chard, half a cup of black beans, and half an avocado to get your daily magnesium needs met. So easy!
- Reduce exposure to BPA – Bisphenyl-A is a chemical found in many plastics, canned food linings, and even in receipts. There are actually a couple of recent studies that show women with PCOS have elevated levels of BPA in their blood. I doubt this is a coincidence. You have complete control over the plastics you come in contact with so choose products and foods wisely.
- Acupuncture – I am a huge proponent of acupuncture for reproductive health. I know many women who have regulated their cycles and gotten pregnant after introducing acupuncture into their wellness and healing regimen. I highly recommend acupuncture before trying any major medication to address your PCOS symptoms. One session a week is a great place to start. Or, if you can’t get to an acupuncturist or you don’t like needles, Aimee Raupp (fertility acupuncturist extraordinaire!) has a free Fertility Enhancing Acupressure Guide which you can do from home.
If you were to look at what the medical industry has to say about PCOS, you would think it was an unavoidable, incurable, genetically contracted disease. But if you look closely at the claims they make to support this, you’ll see that the scientific evidence suggesting that genetics plays the predominant role in PCOS is not necessarily the case.
This is because families share a lot more than just genes, right? They also share an environment, sometimes a similarly active or inactive lifestyle, and most importantly in this case, dietary habits. To conclude that genetics is the main cause of PCOS simply because family members are more likely to have it ignores all of these other things that families share and completely misses the root cause of the issue.
When a woman hears that she has been diagnosed with an incurable disease that was handed down to her, her options for treatment immediately become limited. She feels that, if her disease was out of her control, then so must be her recovery. The only option is to place her future in the hands of her doctor and the pharmaceuticals he prescribes and hope for the best. And we all know how well that usually works!
In a condition like PCOS where a woman’s lifestyle (including daily stressors) and food choices are such a huge component, I urge every woman to at least consider all their options before resorting to invasive medical procedures.

16 thoughts on “The PCOS Protocol: The Main Cause of PCOS and Tips to Treat It Naturally”
Pingback: Common (But Surprising) Causes of Irregular Periods - Nicole Jardim
Pingback: How Ovulation Works And Why It’s So Important - Nicole Jardim
Pingback: 7 Surprising Reasons Women Lose Their Hair - Nicole Jardim
Pingback: The Best Time In Your Cycle to Test Progesterone - Nicole Jardim
I am 22 years old, vegetarian, a health nut, take a supplement to rid my body of DHT and unhealthy estrogens and still have PCOS lol. I am at a healthy weight, I eat raw vegetables, wild rice and beans for virtually every lunch/dinner. I am an NCAA athlete so my activity level is very high. What else am I supposed to do because none of it has changed my symptoms.. and I already do most of this..
Pingback: Hormonal Imbalance It All Starts with the Adrenals | Better Periods in 2012
Hi Nicole,
Great article, very informative. I’m almost positive my girlfriend has PCOS. She lives on a small Island where the medical treatment is not that great. She hasn’t been officially diagnosed with this condition, but she does have cysts on her ovaries and her harmones are all out of whack. At her last visit her Dr told her her cysts were getting bigger and removal of her ovaries is imminent and should happen sooner rather than later. She hasn’t been back to the doctor since. That was last nov.
I’m curious, what is the definitive test that diagnoses this condition? And what tests should be performed to figure out what needs to be done? I know sugar is one of the main ones, but are there others and do you have to trend them throughout the month in relation to ovulation?
Myoinositol reduces insulin levels and helps with pcos. Many women have regular periods because of it.
Yes, absolutely. I’ve used it very successfully in my work with women who have PCOS.
Hi I tried to click on the link to your Facebook but it just froze up. I’ve been dealing with PCOS my entire adult life. Now I’m having issues with critically low vitamin D levels, B12 levels and I know that my thyroid gland was damaged during an anterior cervical discectomy. I had regular periods and I have not had one at all since the end of April beginning of May of this year. My surgery was December 29th 2016, with multiple complications. I have had little to no so-called menopausal symptoms. My period’s just decided to stop. Something is not right at all! I do not have vaginal dryness at all, nor am I having night sweats, and my libido is just fine. I am not however, sexually active. I am 48 years old, but I was not near menopause before any of this. Looking forward to joining your Facebook group and keeping up with your posts on these topics!
This blog post gave me a lot of comfort, thank you Nicole. I was recently diagnosed with PCOS after having issues conceiving and then miscarrying twice. My doctor of course told me there is no cure but deep down I knew it was years of binge eating and sugar addiction that was causing my hormonal imbalances. The Info on your site has pointed me in the right direction and given me inspiration to make changes to my diet.
I’m so afraid that I have permanently damaged my body beyond repair. Is that possible? Or even after years of too much sugar can I correct my hormone problems? How long does it take for insulin levels to be corrected?
Thanks!
I wonder why there are so less comments. a huge thank you…!!!I think that can lead me to a happier life :). despite the beans ( I cant eat them…I dont like them at all…) I hope to get free of the PCO….is any sugar allowed ? I mean there cant be a life without any swiss chocolate, I would deny my country ;).
cheers
There are a lot of incredible questions on here, but it’s so much easier to get clear answers in our Know Your Flow Facebook group. Just paste the following link into your browser:http://tinyurl.com/pkflo6r
There are tons of women in there who’ve had similar experiences and it’s much more private. I also have a free Period Survival Guide for you here: http://tinyurl.com/nh7y55g
Thanks.
PCOS another “disease” that is “cured” by simple mostly non-medical means. Gee is good health that easy?
Good article; the dangers of excess insulin extend to us males also.
http://healthyprotocols.com/2_insulin.htm
This is a great blog post, Nicole! Thank you so much for the simple and clear explanation! I completely removed sugar as well as fructose from my diet and I stopped getting tired after each meal. I found out that even a small apple can cause problems for me. I must be super insulin-sensitive. Anyway, keep up the good work!!!! Much love.
Hi Iga, your welcome, I’m so happy this post resonated with you. I like explanations to be really broken for me so I also try to explain things that way too! 🙂 I agree that even an apple can have a negative effect on some women. I’m a huge fan of eating protein with fruit, nut butters with apples, almonds or walnuts with berries. And of course staying away from the tropical fruits like pineapple and mango – or at least having them in really small amounts. xoxo