Raise your hand if you currently feel stressed out.
Tragically, in today’s society, running around like a chicken with our heads cut off is the norm. We live in a world where busy-ness is glorified and stress equals success. As my girl Dr. Carrie Jones said in a post on stress recently, there is no award for being the busiest!
What constitutes stress to the body?
Women are adaptable creatures—we adapt to our surroundings and environments quite flawlessly. Which, while a great skill to possess in the workplace or even for our own survival, does not always bode well for our menstrual cycles and fertility.
Let me explain: Because we’ve learned to “adapt” to all of the different forms of chaos in our lives, most of us don’t even realize how much tension is building up in our bodies day after day by seemingly small things.
Traffic jams, blue light exposure, family drama, low self-esteem, excess caffeine, processed foods… the list could go on forever.
Even our coping mechanisms are potential stressors! The two glasses of wine you had last night, for example (sorry, don’t shoot the messenger), or how about the intense spin class you took at 5am in lieu of an extra hour of shut-eye?
Yep, our bodies consider that stress, too. Let’s face it: We aren’t running from lions anymore, but with the constant overstimulation on a day-to-day basis, we might as well be.
To make matters worse, women’s bodies in particular are highly susceptible to the stressors of modern life, and this is where we start seeing hypothalamic-pituitary-adrenal (HPA) axis or adrenal dysfunction arise. And I’m sure you can guess what part of our biology takes the hardest hit…
That’s right, our HORMONES, particularly our beloved sex hormones. Keep reading to learn about how our hormones and menstrual cycle are affected by adrenal dysfunction and what we can do about it.
How Adrenal Dysfunction Affects the Reproductive System
First, a word on the HPA axis: The hypothalamic-pituitary-adrenal axis coordinates our body’s stress response—the brain signals the adrenals to secrete hormones like epinephrine and cortisol in a perfectly orchestrated pattern that helps us respond to occasional stressors. (The keyword being occasional.)
When we’re in a state of chronic stress, however, this pattern can easily become disrupted, resulting in adrenal hormone dysfunction. But how does this dysfunction mess with our reproductive systems, exactly? It’s a bit of a top-down domino effect…
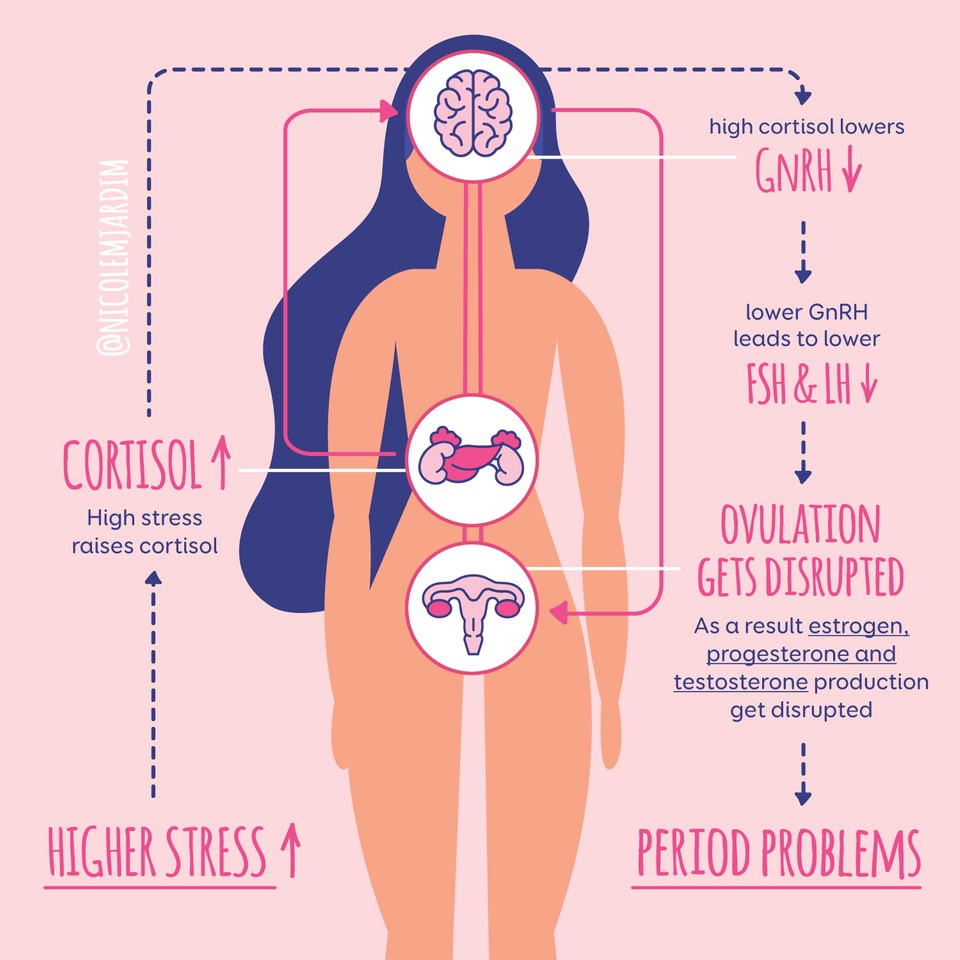
- High cortisol brought on by stress dampens the hypothalamus’s GnRH secretion, which is responsible for triggering the pituitary to release FSH and LH, indirectly telling the ovaries to decrease their production of estrogen, progesterone, and testosterone (1, 2, 3).
- Similarly to its effect on GnRH, cortisol also directly inhibits the production of FSH and LH in the pituitary in a further attempt to thwart the chance of ovulation and potential pregnancy (1).
- As a result, over time the production of estrogen, progesterone and testosterone goes a little haywire, thus disrupting the entire menstrual cycle.
Can you see now how ongoing activation of our body’s stress system and higher levels of stress-related hormones are directly linked with anovulatory cycles or irregular ovulation? We’re talking irregular periods or hypothalamic amenorrhea (HA) in some women, or heavier periods and spotting in others (4).
But that’s not all, not by a long shot…
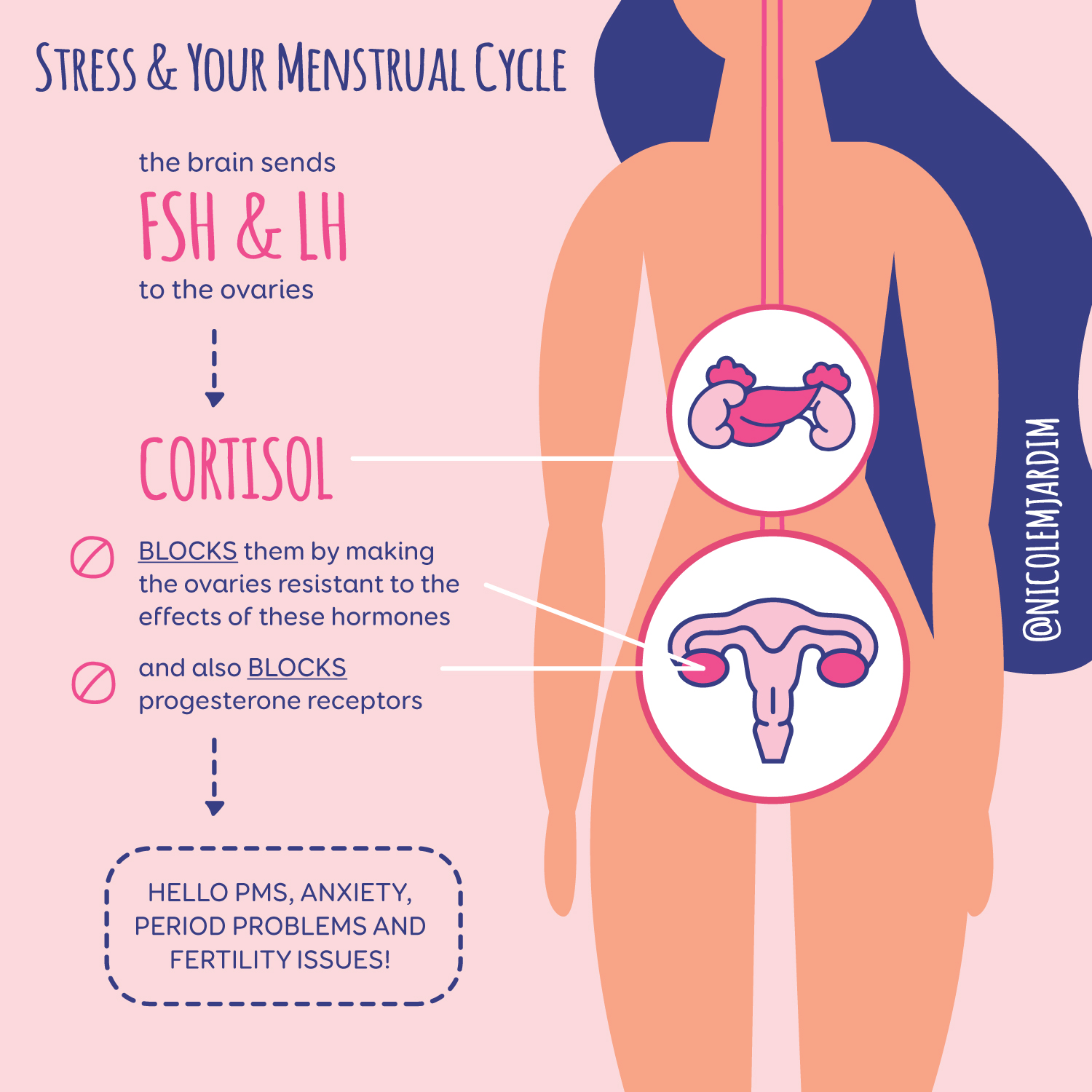 If by some miracle, enough FSH and LH make it to the ovaries, cortisol actually BLOCKS them by making the ovaries resistant to the effects of these hormones (5).
If by some miracle, enough FSH and LH make it to the ovaries, cortisol actually BLOCKS them by making the ovaries resistant to the effects of these hormones (5).
As if that wasn’t enough, cortisol also blocks progesterone receptors, basically mimicking progesterone deficiency in the body. (Hello PMS, anxiety, period and fertility probs!)
And finally, in one study done on women undergoing IVF, it was found that cortisol was higher in the follicular fluid of eggs that were not fertilized and lower in eggs that were successfully fertilized, indicating that higher levels of cortisol may actually hinder egg maturation in your ovaries (6). Oh, jeez!
So what does all this mean?
Put simply, when we’re facing what the body considers to be an emergency situation, the last thing it wants to do is procreate (5)! And since our bodies evolved a looooong time ago, it doesn’t really grasp the difference between your daily 5-mile jog and coming face-to-face with a saber-toothed tiger.
Stress and the Thyroid
Were you aware that cortisol can also greatly hinder thyroid hormone production as well? Here’s how it all plays out:
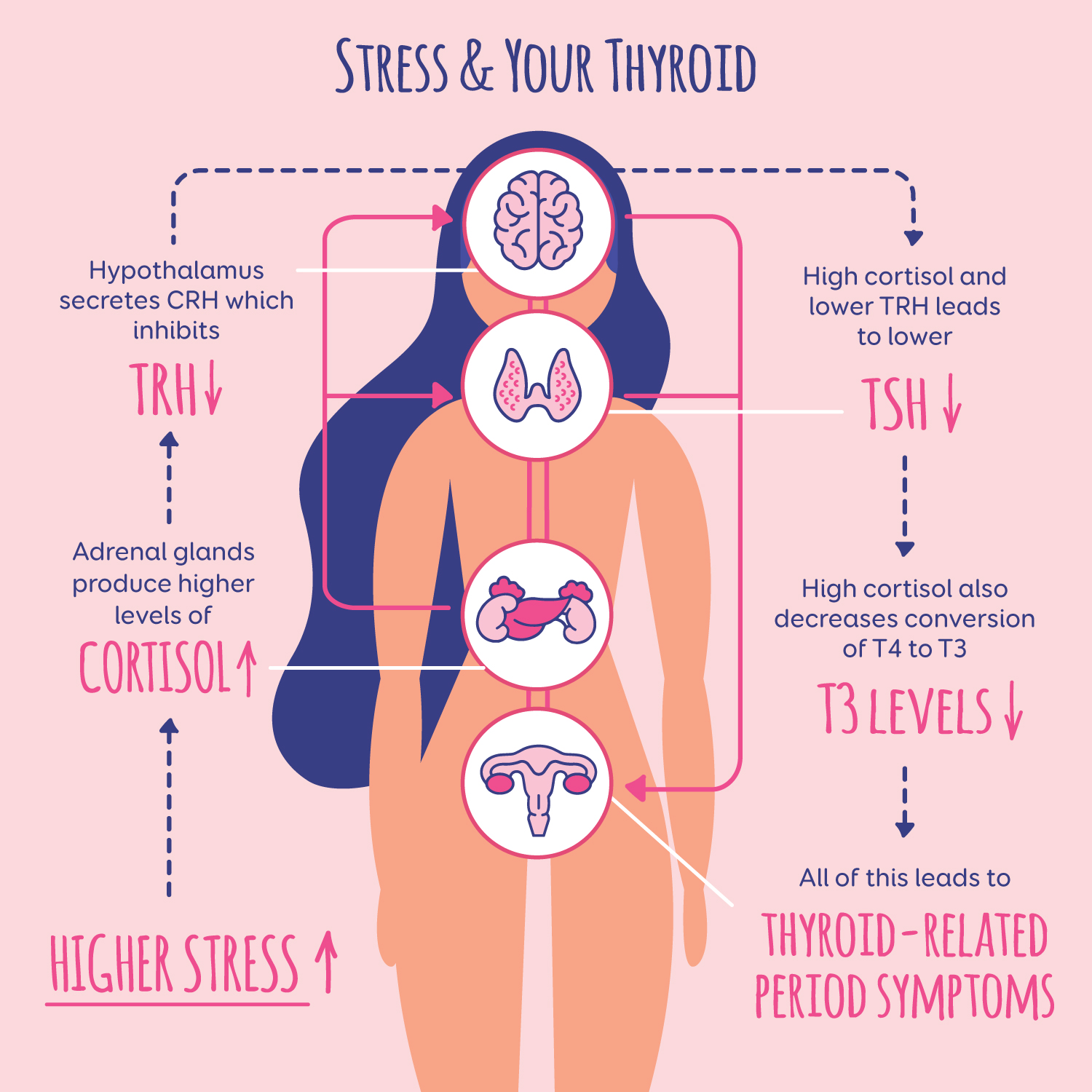
- Similarly to the ovarian hormones, CRH (a hormone released in response to stress) inhibits thyrotropin releasing hormone from the hypothalamus, inhibiting TSH production from the pituitary. Rising cortisol levels directly lower TSH production as well (7).
- Elevated cortisol suppresses the deiodinase enzyme, which is critical for converting T4 to T3. When the conversion of T4-to-T3 decreases, you don’t have as much of the active form of thyroid hormone that your body needs to function at its best. (Hello, hypothyroidism!)
- In times of stress or illness, our body converts more T3 into something called Reverse T3, which is meant to conserve energy and can lead to or even worsen hypothyroidism symptoms (7).
- Cortisol also raises blood sugar and can lead to insulin resistance, a condition that damages the thyroid cells and worsens thyroid disorders.
Want to learn more about how thyroid disorders can impact your period and fertility? Read my post on the subject here.
The thyroid and sex hormones aside, sustained high cortisol is also linked to high blood pressure, diabetes, increased belly fat, brain changes, depression, insomnia, and poor immunity (8, 9).
Bottom line: Sustained high cortisol is NOT conducive to healthy hormones, a normal period, or optimal fertility!
What to Do About High Cortisol or Adrenal Dysfunction
Okay, so you’ve had your cortisol levels checked (I recommend this test from Lets Get Checked—use code Hormones20 for 20% off!) and the results were out of range. Now what? Before you start researching all the things you need to do in order to heal, take a breath and consider this:
Many women I work with who either aren’t ovulating or are experiencing sporadic periods due to high stress feel as if their bodies have betrayed them. I sense frustration and resentment when they tell me that they’re doing everything perfectly to optimize their health—eating well, exercising, sleeping 8 hours a night, etc.—but their hormones just won’t cooperate.
What many women might not get right away is that this effort to be “perfect” could be what’s holding them back from fixing their period in the first place. In order to regulate ovulation and restore fertility, we have to address both real and perceived stress so that our bodies can feel safe again.
Sometimes, this means more than simply taking up yoga or meditation. For some, it could look like scaling back on work (if possible), mending a broken relationship, delegating household chores, stepping down from social obligations, breaking free of restrictive eating patterns, or simply doing the emotional work to free themselves of resentment and fear. For others, finding a way to rethink and react differently to stress is key. It all depends on what is causing your body to hold onto the most tension.
It’s pretty much across the board, however, that once women understand that their body is actually working for them—and not against them—they can move out of the place of disempowerment and blame and start on the road to healing.
That said, head on over to this blog post to get some practical tips for reducing cortisol!
************
Sources
- https://www.ncbi.nlm.nih.gov/pubmed/20595939
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC539265/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4166402/
- https://link.springer.com/article/10.1007/s40750-014-0004-2
- https://www.ncbi.nlm.nih.gov/pubmed/8334750
- https://www.ncbi.nlm.nih.gov/pubmed/1471451
- https://www.ncbi.nlm.nih.gov/pubmed/12377295
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462413/
- https://academic.oup.com/jcem/article/94/8/2692/2596309

2 thoughts on “How Stress Affects Your Menstrual Cycle”
Pingback: Pandemic Periods - Nicole Jardim
Pingback: Low Progesterone: Why it happens and what you can do about it - Nicole Jardim