I first heard about endometriosis in my early 20’s when a doctor suggested I might have it. At the time I had debilitatingly painful periods that made me want to curl up into a ball under my desk each month. In fact, under my desk or on the couch in the production office (I used to be a freelance production coordinator on TV commercials in my former life), was where my production manager would often find me!
This doctor was clearly ahead of the game, but there wasn’t much she could offer me besides the pill. I’d been there, done that, so the pill was not an option for me at that point. In fact, in the five years I was on it, it had just masked all the symptoms I’d been experiencing, and now I felt like I was back to square one. Ugh.
I’ll share further down what I did instead of succumbing to the pharmaceutical push (because as you can imagine, that was certainly not the last time it was offered as a panacea for all my period woes).
Alarming Endometriosis stats
- Endometriosis is estimated to affect approximately one in ten women of reproductive age, which is approximately 176 million women & people who menstruate in the world.
- Studies have shown a delay from 3 to 11 years between the onset of symptoms and the final diagnosis of endometriosis. With an average of 9.28 years before receiving a proper diagnosis!! [2] (Um, hello! This is just not okay. Women’s health concerns need to be taken way more seriously. But don’t get me started on gender bias in medical care…I think a post on the topic is in order).
- Up to 30% – 50% of women with endometriosis may experience infertility. Sadly, it’s one of the top 3 causes of infertility.[3]
- One study found the prevalence of endometriosis in adolescent girls with pelvic pain to be close to 50%, whereas others estimate the number to be roughly 70%. This condition starts when we are young, and we have to intervene as early as possible.
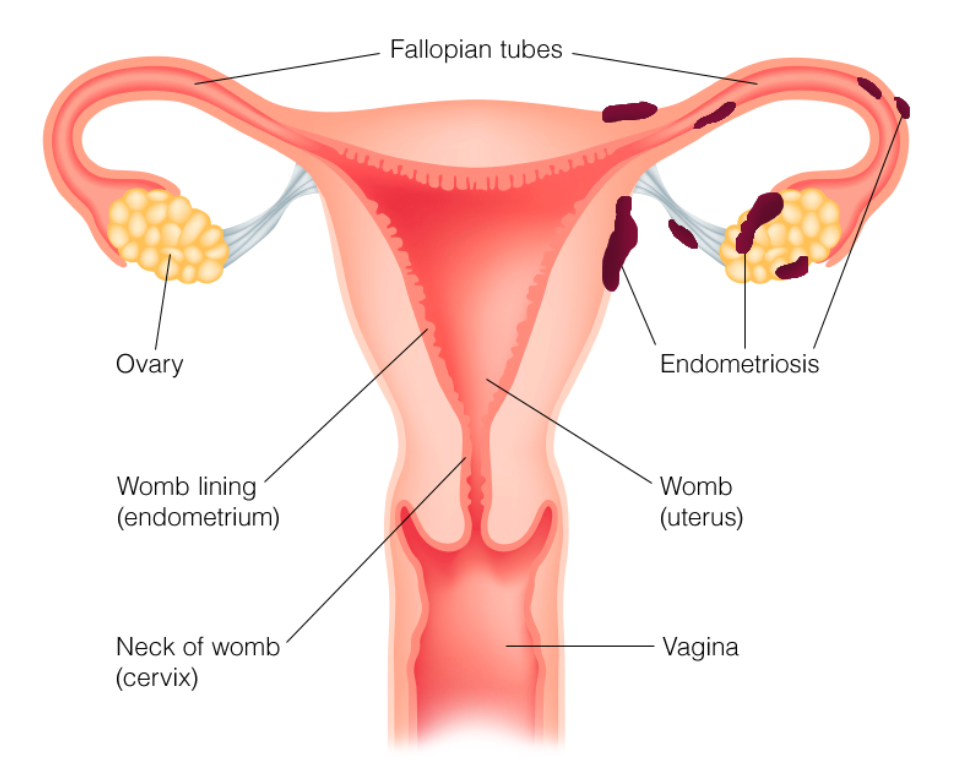
What is Endometriosis?
Endometriosis is a complex inflammatory disease in which tissue that is similar to the kind of tissue that grows in the uterus grows outside of the uterus (instead of just on the inside). This tissue responds to the hormone fluctuations that govern the menstrual cycle in the same way it would if it were in the uterus, building up each month before the period (to prepare for possible implantation of a fertilized egg), and then breaking down when the body signals that it’s time to shed this lining.
Endometriosis is typically non-cancerous and can cause A LOT of pain throughout the menstrual cycle, not just at menstruation.
The endometriosis growths and lesions are commonly found on organs in and around the pelvis like the fallopian tubes, the surface of the uterus, and the lining of the pelvic cavity. Endometriosis can also spread further into the abdomen though, affecting the intestines, the bladder, and the rectum. In rare cases it can even be present in the lungs!
The presence of this endometriosis tissue leads to a chronic cycle of inflammation that gets worse over time. This is because the body doesn’t recognize it, and is constantly sending it’s little immune system foot soldiers to try and address it.
These immune system soldiers contribute significantly to the inflammation as they try to manage the situation and repair the tissue
This leads to the formation of scar tissue and adhesions around the endometriotic tissue, which can cause a whole host of other issues – chronic inflammation, an increasingly abnormal immune response and even more scarring.
So yes, you guessed it – symptoms can worsen over time for many women. However, there are countless women (20-25% of them to be exact) who don’t even realize they have endometriosis until they are trying to conceive and lesions are found.
The symptoms of Endometriosis
Depending on the location and severity of the endometriosis tissue, symptoms can vary quite a bit. Since the endometriosis tissue is estrogen-responsive just like the endometrial lining of the uterus, symptoms often correlate with the menstrual cycles.
The most common symptoms include:
- Pelvic pain, usually with menstruation, but some women may experience pain throughout the entire month
- Severe cramping during menstruation can disrupt life for 1 or more days, and don’t typically go away with anti-inflammatories
- Periods that last longer than 7 days (this often correlates with also having adenomyosis)
- Heavy to very heavy menstrual flow (this often correlates with also having adenomyosis)
- Bowel and urinary disorders that include painful urination or IBS-like symptoms. These conditions include vulvodynia, interstitial cystitis and pelvic floor dysfunction[4]
- Nausea or vomiting, especially during menstruation
- Bloating
- Debilitating fatigue
- Depression and anxiety
- Pain or bleeding during sex
- Spotting or irregular bleeding outside of your period, and
- Infertility – it manifests in up to 40% of women with endometriosis.
Causes of Endometriosis
Currently, endometriosis is rather poorly understood by the western medical community, and they have been slow to catch up to the latest findings on this condition.
Researchers have concluded that endometriosis has almost all the hallmarks of an autoimmune disease, and has been found to occur in conjunction with other autoimmune conditions like multiple sclerosis, rheumatoid arthritis and inflammatory bowel diseases (including Crohn’s and ulcerative colitis) [5].
So this means there is definitely a connection between endometriosis, overall inflammation and immune system dysfunction. Digging even deeper, inflammation is connected to our gut function and liver health (the liver’s ability to detox effectively), because gut and liver health play an important role in autoimmunity and the development of autoimmune disease.
Additionally, research shows that while hormonal imbalance is not at the root of this painful condition it massively exacerbates it, with excess or unopposed estrogen being at the forefront. In other words, hormonal imbalance can make it worse, but doesn’t cause it.
Genetics also play a role as it’s been found that women who have a close relative with the condition are 7 to 10 times more likely to get endometriosis. In female twins, there is a likelihood that both will get the condition, especially if they are identical.[6,7] Other factors that have been linked to the development of endometriosis include alcohol use, which can increase estrogen in the body and decrease the liver’s detoxification function, and low body weight.[8,9]
With regard to this, there are theories that suggest implants of the endometriosis tissues happen on the external surfaces of the pelvic organs during embryonic development, and then become “active” as puberty begins and the estrogenic environment changes, or through xenoestrogen exposure.
There is also evidence to suggest impaired methylation status in women with endometriosis due to genetic mutations. What this means is that in women with endo, the body is over-responding to estrogen which encourages growth of the endo lesions, while progesterone receptors are being silenced and thus becoming unresponsive to progesterone, which would normally balance out the strong influence of estrogen. As you know, estrogen feeds endometriosis lesions.
There has been a longstanding belief that something known as retrograde menstruation is also a cause of endometriosis. Normally, menstrual blood should flow from the uterus out of the body, but instead of the blood flowing out of the body through the vagina, the endometrial lining flows backwards through the fallopian tubes and into the abdomen. Here’s the thing, retrograde menstruation is associated with endometriosis, but not every woman who experiences retrograde menstruation has endometriosis. So, if you experience retrograde menstruation, it does not automatically mean you have endometriosis.
How Is Endometriosis Diagnosed?
Endometriosis is difficult to diagnose. According to the study Invasive and non-invasive methods for the diagnosis of endometriosis, “imaging has limited utility in the diagnosis of endometriosis, as it lacks adequate resolution to identify adhesions or superficial peritoneal implants. Ultrasound is cheap and easy to perform, but user-dependent; MRI is more accurate but considerably more expensive. A CT scan of the pelvis does not visualize pelvic organs well, so it is not useful in the diagnosis of endometriosis. An important role for the CT scan with contrast is to detect ureteral involvement and possible renal insufficiency.”
There are new developments in the use of these imaging techniques for diagnosis. I’ve interviewed Dr. Mathew Leonardi on the podcast and we talk about his pioneering techniques using ultrasound for diagnosis.
However, for the most part, using imaging is still just one piece of the diagnosis puzzle and there may need to be other diagnosis criteria for you personally.
Exploratory laparoscopy surgery is still currently considered to be the only fully viable method to diagnose or rule it out. Because there is not a great non-invasive widely available alternative for diagnosis, women can wait for up to twelve years to get a proper diagnosis! What often happens instead of a diagnosis is women are prescribed the pill, pain medication and antidepressants, and sent on their way.
FYI – the pill does not slow down or stop the growth of endometriosis. The tissue can continue to grow while someone is on the pill.
Is there a cure for Endometriosis?
There is currently no known cure for endometriosis, but there is a lot that can be done. I break it down into three components.
#1. According to the top endometriosis clinicians, the most important first step once endometriosis has been confirmed, is to find a SKILLED excision surgeon to remove the endometrial lesions and any scar tissue. While this surgery isn’t necessary for relieving pain in every case, it is one of the best ways to stop the progression of the disease, improve your quality of life, and preserve your future fertility.
A good surgeon can usually remove everything in one go, but there are instances where multiple excision surgeries are required – usually if a woman has had previous surgeries or if the disease has had a lot of time to progress. In addition, hormonal suppression is used in conjunction with surgery (the birth control pill or Lupron are often used, but there are side effects to consider. Speak with your doctor about this).
Here are some resources:
- Check out Dr. Jessica Drummond’s in-depth post on endometriosis, and how to find a skilled surgeon. She is an incredible endometriosis expert and offers programs for those with the condition.
- Check out the Endometriosis Foundation of America for even more helpful information.
#2. Additionally, women with endometriosis should also see a Pelvic Physical Therapist before, and after surgery to provide the best possible outcome for their recovery.
#3. I’m not an expert on surgery or hormonal suppression (so I can’t speak extensively about it), but I am an expert on nutrition and lifestyle adjustments, which is the third component of a well-rounded approach to endometriosis. 🙂
The goal when it comes to endo is to try and mitigate its symptoms by supporting the immune system (so it can work properly) and addressing inflammation. A natural approach that removes endocrine disruptors, and supports detoxification of estrogen has been extremely helpful in my practice.
More resources here in this article.
Making the case for optimal gut health if you have Endometriosis
The health of the GI tract is connected to endometriosis. Here are two reasons why…
Lipopolysaccharides & Leaky Gut
Lipopolysaccharides (or LPS) are endotoxins that come from the outer cell walls of unfriendly bacteria, also known as gram-negative bacteria. When the GI tract is out of balance and a person has leaky gut, LPS can travel across the gut barrier and enter the body. These toxins can have far-reaching effects – particularly on the immune system.
In combination with estradiol, LPS can promote pelvic inflammation and worsen endometriosis.[10] One study found that 80% of women with endometriosis have SIBO, and another suggested that the health of the intestinal bacteria played a critical role in the development and progression of endometriosis.[11,12]
Additionally, endometriosis can directly affect the GI tract, so it goes both ways. Prostaglandins, which are released during menstruation by the uterus and the endometrial lesions, affect the smooth muscle of the bowel and cause symptoms such as intestinal cramping and diarrhea. The endometrial cells can even invade through the wall of the intestines. This interferes with the gut’s ability to keep waste products moving, resulting in SIBO, yeast overgrowth, and bacterial imbalance, all of which will only worsen endometriosis as I just said.
Histamine Intolerance
Histamines are chemicals that are stored in immune cells known as Mast Cells, and are involved in nerve transmission and immune response regulation. When Mast Cells are triggered, they release histamines.
When a person has a histamine sensitivity, certain foods or environmental stimulants can cause a host of symptoms including: flushing, sneezing, itching, hives, headaches, wheezing, swelling, anxiety and difficulty sleeping.
Interestingly, in women with endometriosis, mast cells are present in much higher quantities in the endometriosis tissue, than in healthy tissue of women who don’t have endometriosis.[13] As mentioned earlier, there is a correlation between an abnormal immune response, specifically a hyperimmune response and endometriosis.[14]
While genetics and certain foods can certainly play a role in histamine sensitivity, gut dysbiosis makes things much worse. People with leaky gut or small intestine bacterial overgrowth (SIBO) are much more prone to histamine sensitivity.
This means that people with endometriosis need to support overall gut function and may want to experiment with avoiding histamine triggers.
Check out my colleague Jessica Duffin for more information on the connection between endometriosis and SIBO.
Solutions For Managing Endo Naturally
I never did the laparoscopic surgery to determine if I had endo, but I did a complete overhaul of my life in order to get my period pain under control. It wasn’t easy – I changed careers, upgraded my diet, lifestyle, and supplement regimen, and even moved to a place that made me happier!
And that brings me to my TOP SEVEN recommendations to help YOU manage endometriosis naturally.
#1 Curcumin (a powerful ingredient in turmeric)
In addition to being an incredible anti-inflammatory/brain boosting/cancer-preventing powerhouse, curcumin also prevents the growth of endometriosis cells by inhibiting the production of the hormone estradiol.[15] I recommend a curcumin supplement like this one. You can find it in the Painful Periods Supplement Protocol in my supplement dispensary. You’ll get 15% off on all orders, but you have to create an account to purchase supplements.
#2 Omega-3 Fatty Acids
Add in cold-water, fatty fish to your diet, such as salmon, mackerel, herring, and sardines. Or supplement with 2 capsules of this omega-3 fish oil a day. I’ve written here about the connection between omega-3’s, inflammation and physical pain.
#3 Avoid or limit histamine-releasing foods
Try limiting intake or cutting these out completely for 4 weeks to see if there is a reduction in your symptoms.
- Fermented, cured, or soured foods, such as yogurt, luncheon meat, pickles, and sour cream
- Aged cheeses, such as cheddar and goat cheese, and smoked fish
- Citrus fruit and dried fruits such as apricots and raisins
- Alcoholic beverages, especially wine and beer
- Certain nuts, including walnuts, peanuts, and cashews
- Avocados, eggplant, spinach, tomatoes, chocolate, and dairy
I am also a big fan of quercetin, a flavonoid which works like an all natural anti-histamine – stabilizing the effects of histamines released from mast cells. It also doubles as a leaky gut and pain reliever. I like Pure Encapsulations Quercetin and the recommended dosage is 500mg a day for 8-12 weeks.
#4 Blood sugar balancing for the win
If your blood sugar is consistently unstable, then it’s contributing to inflammation in your body. Long-term inflammation = pain. The goal is to eat a balance of protein, carbs, fat and fiber so your blood sugar doesn’t spike and crash all day long. This translates to more stable energy (no crashes mid-morning or mid-afternoon), more stable moods less drama, better sleep, beautiful skin and hair (yes sugar messes these up too), and waaaay better periods!
If you want to get a full morning, lunch and dinner protocol along with the exact steps you need to take to reclaim your energy, sparkle and inner happy girl (TODAY), then check out Week #2 in the protocol of my book Fix Your Period.
#5 Castor Oil Packs
Castor oil is derived from the seeds of the Castor Oil plant and has been used by many cultures for centuries to promote healing, specifically reproductive system healing. To learn more about this amazing pain remedy, read my blog post about it and download my free castor oil pack guide.
#6 Support your liver’s ability to process estrogen
Each day eat a cup of cooked cruciferous veggies like broccoli, kale, collards, cabbage, and brussels sprouts, which are nutrient powerhouses that will help support the liver’s estrogen detoxification capacity.
You may also want to add a liver-supportive supplement. Some of the most potent liver supportive ingredients include milk thistle, N-Acetyl Cysteine, Alpha Lipoic Acid, turmeric, artichoke extract, broccoli sprout concentrate or sulforaphane, and methionine. Overall, these compounds act as potent antioxidants, they reduce inflammation in the liver and they support phase 1 and 2 of liver detoxification. My favorite product is Pure Encapsulations Liver GI Detox.
#7 Avoid exposure to damaging chemicals and xenoestrogens
Polychlorinated and brominated chemicals, like PCBs and flame retardants, are harmful to the liver. These are present in drinking water and many foods. Other environmental toxins such as BPA and other plastic softeners like phthalates can artificially increase estrogen levels. Dioxins, which are bleach byproducts should also be avoided because they contribute to endometriosis progression.[16]
- Avoid plastics including water bottles and food packaging, BPA-coated receipts and plastic flip flops. And ditch anything with the word “fragrance” in the ingredients. Try these silicone food storage containers, and this awesome plastic wrap alternative.
- Include as many organic and locally sourced foods in your diet as possible.
- Consider installing a high quality home water filtration system, or start by purchasing a drinking water filter like a Berkey Countertop Filter and a shower filter.
- Use only natural home cleaning products and personal care products (I am currently in love with Beauty Counter skincare and makeup products!). And to avoid dioxin, switch to organic cotton tampons, pads, or period underwear.
References:
- Rogers PA, et al. Priorities for endometriosis research: recommendations from an international consensus workshop. Reprod Sci 2009;16(4):335-46.; Adamson GD, et al. Creating solutions in endometriosis: global collaboration through the World Endometriosis Research Foundation. J of Endometriosis 2010;2(1):3-6
- http://www.ncbi.nlm.nih.gov/pubmed/12790847
- http://www.asrm.org/uploadedFiles/ASRM_Content/Resources/Patient_Resources/Fact_Sheets_and_Info_Booklets/EndoDoesItCauseInfertility.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4432718/
- https://www.ncbi.nlm.nih.gov/pubmed/24807511
- https://www.ncbi.nlm.nih.gov/pubmed/22330229
- https://www.ncbi.nlm.nih.gov/pubmed/26247027
- https://www.ncbi.nlm.nih.gov/pubmed/21620779
- https://www.ncbi.nlm.nih.gov/pubmed/8488967
- http://www.medpagetoday.com/obgyn/generalobgyn/39127
- https://www.ncbi.nlm.nih.gov/pubmed/25355803
- https://www.ncbi.nlm.nih.gov/pubmed/9660426
- https://www.ncbi.nlm.nih.gov/pubmed/26901277
- https://www.ncbi.nlm.nih.gov/pubmed/17007852?dopt=Abstract&holding=f1000
- https://www.ncbi.nlm.nih.gov/pubmed/15727565
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3941414/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2875884/

16 thoughts on “Living With Endometriosis: The Real Causes + Natural Solutions”
Hi, thank you for this article. I have Endo since so many years. Anyway, I am reading about turmeric everywhere as a key part of the solution. The problem is that I have had for years iron deficiency (lower than minimum). I am finally getting it on track. However I read that turmeric strongly affec the iron intake (up to 80%). 🙁 so what is an effective alternative? Ginger?… thanks
Hi there,
I just had my laparoscopy after suffering for about 20 years. Since the operation, my gut has cleared up tremendously as I was diagnosed with Sibo about 5 years ago. But the symptoms like bloating and constipation are starting to creep in again, which I’m so upset about. I thought with the endo removed, my gut might be restored to a better condition and the SIBO would dissapear? Is that wishful thinking?
Thankyou
Yas
Keep doing what you’re doing – it’ll provoke debate, disagreement and annoyance in some, but for others it could be life-changing. I was diagnosed in 2013 and chose to take a holistic route rather than surgery/hormones. Finally found a supportive GP and became my own medical researcher! Cleaning up chemicals in the home (makeup, cleaning, cooking & containers) and going organic had the most impact on my symptoms. Some supplements help (I find resveratrol useful to help handle oestrogen levels, serrapeptase seems to encourage loss of endo tissue at period time for me too) – but I’ve just moved house and had a hyper-histamine response, so I’ll look at quercetin. Thanks! Fingers crossed it’s a stress response rather than I’m allergic to my beautiful new home 😉 Look at me – cracking a joke when endo had me suicidal 2yrs ago. Keep doing what you’re doing – it could be life-changing x
I have endo and was dx via laparoscopic surgery and excision. The only thing I haven’t been able to find online or from a doctor is the if/when will the endo come back after it’s been removed and what happens next?
(At age 20 It took about 6 months from my symptoms to get out of control, vomiting for almost 2 weeks and having unbelievably painful periods – which I was given anti nausea and pain meds to help with and sent on my way – to finally diagnosis and surgery. But I am pretty sure I had been experiencing a lot of other symptoms for years before that would continually be written off and ignored – especially bc I was in college)
Sara, there is no guarantee the endo won’t come back but you have A LOT of control over the diet and lifestyle factors that contribute to it so you should work with someone who can help you specifically with this. A naturopath, health coach or functional med doctor would be a good start.
Sam-e solved my cramps, PMS and depression 🙂
That’s awesome to hear Bianca!! It’s a great feeling when you find a solution that works 🙂
Let me just point out that a lot of endometriosis sufferers who experience IBS-like symptoms, or who actually also have IBS, can’t tolerate most cruciferous vegetables.
HI Alexandra, thanks for your comment. I recognize that functional gut disorders like IBS and IBS-like symptoms have a big impact on overall health and quality of life. I think it is important to consider factors that contribute to IBS or IBS-like symptoms. For instance, a low FODMAP diet has been demonstrated to reduce functional gut disorder symptoms in about 75% of people, because most people with IBS have FODMAP intolerances. https://www.ncbi.nlm.nih.gov/pubmed/20136989
Understanding how foods high in FODMAPs affect the gut and knowing how to eliminate them may be the key to getting IBS symptoms under control for some women. None of the dark leafy green cruciferous veggies are high in FODMAPS 🙂
Additionally, emotional and physical stress are also known to be contributing factors to the development of IBS, with a disturbance of gut bacteria being a likely factor. causative factor – stress alters gut flora significantly, so it is super important to have adequate stress-mitigating practices in place. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202343/
So these are two options for women with endometriosis to help address IBS symptoms. Hope this is helpful.
Thank you SO MUCH for this excellent post. I was diagnosed with endo 4 years ago via a laparoscopy. The endo is now back, my lower abdomen is hard and I don’t want to be ‘treated’ with the combined pill anymore, clearly it doesn’t work.
In addition to endo, I have severe bloating which I’ve had since I was a kid, but never seen anyone about. Through a series of experiences, I’ve recently become aware of my problem with inflammation and am convinced there is a connection between my gut/digestion/bloating and the endometriosis/inflammation. I recently realised my severe reaction to insect bites is histamine intolerance.
I’ve looked into naturopathy and functional medicine so it’s reassuring to see you mention those. The problem is, it’s hard to find someone in the UK who is an expert in these areas. Can you recommend anyone in the UK?
Many many thanks
Mandip
Very helpful Post Nicole.
Thanks for saying that Shine! 🙂
Great post Nicole!
One question about the Fermented food, what about fermented Cod fish Liver oil such as this one from Green Pasture { https://www.amazon.com/Green-Pastures-Fermented-Liver-Non-flavored/dp/B004QCMGTG/ref=sr_1_4_a_it/141-1097825-7594928?ie=UTF8&qid=1498177259&sr=8-4&keywords=green+pastures+cod+liver+oil } ?
Would it not be an option for somebody with endometriosis? Would a simple cod fish liver oil such Rosita a better match?
Thank you
Marie
Hey Marie! Great question. I actually think that the extra virgin cod liver oil might be a better option than the fermented cod liver oil if trying to avoid foods that trigger histamine release. Not to say that fermented cod liver oil isn’t great, but it would be better to avoid it in this scenario. You can get the Rosita one here: http://bit.ly/1NZxr0W
Hope this is helpful for you! xo
Great article and so happy to see that you have given some key insights about endometriosis, which typically don’t get shared. Love that you have brought in the liver and the gut health components!
I would say that the histamine correlation is perhaps more of a symptom, rather than a cause. The body reacts in an auto-immune response because of the endometriosis lesions and adhesions. It is an inflammatory response. It is this reaction which will cause inflammatory markers such as mast cells to be high. When uncovering more research on it, you will find that C125 inflammatory markers and immune cells like TCells, NK Cells are either higher or lower than they should be when you have endometriosis. This is normal when the body is in a “hyper-drive” to try and heal.
It is therefore important to address not just inflammation and hormone imbalance but also the auto-immune response with having endometriosis. *There is heaps of cool research on the connection with endometriosis being an auto-immune condition.
Let me know if you would like me to share more of this with you hun. Happy to help 🙂
Hey Melissa! Yes, totally agree with you about the histamine response – I just wanted to point it out because experimenting with removing foods that trigger the histamine response is basically reducing the inflammatory response/immune response –> histamine response and helpful in gut healing. I figure its another way of looking at the overall inflammatory response that some women might want to try. Thanks for all the details info and of course would love to see more research – send it over and we can nerd out. lol xox!