You know that feeling you get when you’re trying to choose a paint color at Home Depot? Yeah that feeling of total bewilderment as you stare at the 437 different shades of yellow. Most of them would probably work in your bedroom but they also each have their own unique, yet subtle qualities so it becomes impossible to choose. AND, when you finally get over that hurdle, you then have to choose the brand of paint along with whether you want eggshell, semi-gloss or flat.
Decisions! Decisions! I liken this paint-choosing process to the task of trying to navigate the vast array of birth control options, methods and brands and how to determine which one (if any) is for you. A daunting mission to say the least!
Unfortunately, in most cases your doctor will make this important decision for you. BUT there is a lot you SHOULD know about what will happen once birth control and your body become acquainted – much more than what that little tri-fold birth control brochure will tell you.
And who are we kidding? That brochure usually ends up at the bottom of your purse and eventually in the garbage (unread) anyways right?
So, why is it that we aren’t more inquiring about what we’re putting into our bodies and how it will affect us? The answer to that is complicated but it starts with the fact that we are not taught, at any age, to be curious about our bodily functions, much less how to decipher what’s going on “down there.”
But that’s why I’m here!
Back when I started taking the pill, I sure wish I had known all that I know now, particularly about side effects. I’m positive I would’ve made a much more informed and educated decision, which would have saved me years of health issues.
Consider this post a little Birth Control 101 for you. While it’s not necessary to get a Masters Degree in this subject it is important to educate yourself. It is your body after all!
Birth Control Options 101
Non-Hormone options
1. Natural Family Planning (NFP) or Fertility Awareness-Based Methods – the best!
Approx Cost: Cheap – the cost of a basal thermometer and the book Taking Charge of Your Fertility and maybe some additional education if you want it.
How it works:
No drugs, no devices, and inexpensive. What more could you want right?
There are a number of fertility awareness-based methods but I recommend using the sympto-thermal method which is most effective. This method includes measuring basal body temperature, observing cervical fluid patterns and cervical position throughout the month. The one I use is the Fertility Awareness Method (FAM) developed by Toni Weschler. Additionally, I recommend the Billings Method which is very similar to the Fertility Awareness Method.
Natural Family Planning is by far the healthiest of all the birth control options because it allows you to be in control of your own body. All it requires is a basal thermometer, a period tracking app or paper chart to record your cycle information and some guidance on how to start. Some women also get formal training from a specialist but that’s not necessary.
Once you get started then you’re the boss of you which is hugely empowering.
Effectiveness:
According to Planned Parenthood, of 100 couples who use the sympto-thermal method correctly for one year, 0.4 (fewer than one) will have a pregnancy. That is just as effective as all of the hormonal birth control methods! Here’s another study for you too.
[1]Dat’s wassup! What else you should know:
Most common question: “Isn’t this just the rhythm method?”
The answer is a resounding no. The rhythm method and/or calendar method is not an effective form of birth control and is based entirely on a woman ovulating on day 14 and getting her period on day 28. The sympto-thermal method is effective because you are measuring your own fertility signs and symptoms and determining the exact days you are fertile. Once you’ve done that you can either avoid sex or use a barrier and/or the withdrawal method.
Added bonus – this method can indicate other issues as well – taking your basal temp can help detect an under-active thyroid, it can tell you whether you are or are not ovulating and if your luteal phase is too short. Charting your cervical fluid can help detect changes that may occur due to an infection, an STD and cervical dysplasia. You can then go straight to your doctor with your findings long before the condition progresses.
2. Withdrawal Method
Approx Cost: Free
How it works:
Commonly known as the “pull-out method” or “pull & pray” (haha), this method is simply the penis being withdrawn from the vagina before ejaculation occurs.
Effectiveness:
This method is surprisingly effective! I know, shocking right? In fact when used correctly it is 96% effective! If used incorrectly it is only 78% effective though. In order to do the withdrawal method properly, the man must pull out before ejaculation and if you decide to go for round two, he must urinate before doing so to get any remaining sperm out of his urethra.
What else you should know:
There have been a number of studies [2] done on whether pre-ejaculate contains live sperm and the evidence overwhelmingly suggests that pre-ejaculate secretions do not contain live sperm.
Hormonal Options
1. Combined Hormonal Birth Control Pill
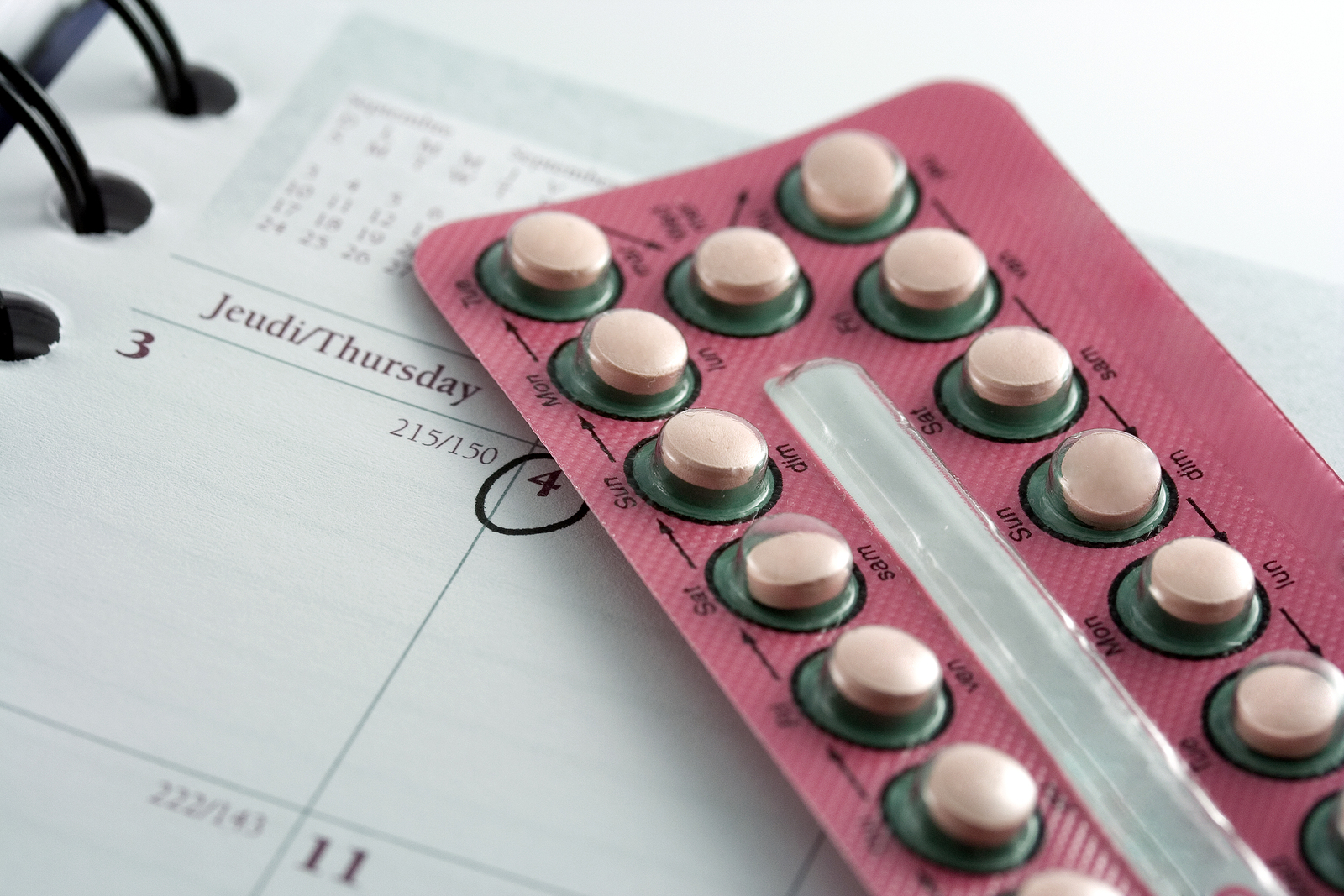
Approx Cost: $15 – $100 per month depending on health coverage and where you live.
How it works:
By far the most common birth control option, the pill releases the hormones estrogen and progestin, which prevent ovulation.
Effectiveness:
- The combined pill is 99.7% effective if taken each day as directed.
- It is only 91% effective if not taken as directed – pills are skipped, etc.
Please note: there is evidence [3] that suggests the pill is not as effective for women who weigh more than 70kg/154lbs and/or have a BMI of 25 and above.
What else you should know:
Unfortunately, the pill comes with a host of undesirable side effects that include, gut/digestive problems, Amenorrhea (no periods), lack of ovulation, mild to severe acne, thyroid dysfunction, mild to severe mood disorders, disruptive food cravings, low to non-existent sex drive, lack of vaginal lubrication, painful sex, thinning of the vaginal tissue and weight gain or inability to lose weight, just to name a few.
Read about clitoral shrinkage here and other things you should know about hormonal birth control here and here.
While there may not be conclusive scientific studies proving all of these side effects, the thousands of women who’ve contacted me in the last four years about their symptoms are proof that the pill can be very harmful. So, proceed with caution.
2. Progestin-Only Pill (Mini-Pill)
Approx Cost: $15 – $100 per month depending on health coverage and where you live
How it works:
This pill is different than the regular pill in that it only releases progestin in the form of norethindrone or norgestrel, (synthetic forms of progesterone). It’s commonly prescribed to women who are very sensitive to estrogen in traditional pills and breastfeeding women because progestin doesn’t suppress milk production. It might also be given to women who are a little older, women who have had breast cancer or other health conditions like high blood pressure, heart disease or history of blood clots.
Effectiveness:
If taken perfectly, that is at the exact same time every day, it is 99.7% effective. If it is not taken at the exact same time every day, then it is only 91% effective. [4]
What else you should know:
The most common side effect is breakthrough bleeding, spotting and irregular menstrual cycles. See above for other side effects that might occur.
3. Birth Control Patch – Ortho Evra
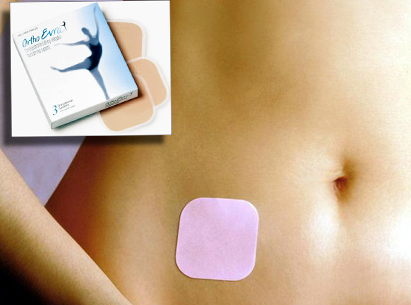
Approx Cost: $0-$80 a month depending on insurance coverage and where you live.
How it works:
The patch was basically created for women who have trouble remembering their daily pill. It is worn on the skin (usually on the arm) and is changed only once per week for three weeks and then the fourth week is patch-free. It also releases estrogen and progestin like the birth control pill.
Effectiveness:
It’s similar to the birth control pill in that it is 99.7% effective with perfect use and 91% effective if not used correctly. As in, you forget to put the patch on after your patch-free week or the patch comes loose and falls off.
What else you should know:
I said it all in the birth control pill section above!
4. Vaginal Ring – NuvaRing
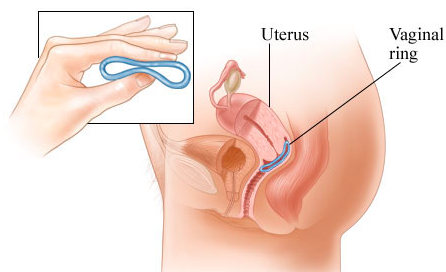
Approx Cost: $0 – $80 per ring/month depending on insurance coverage and where you live.
How it works:
This device is worn inside the vagina and releases estrogen and progestin, the same hormones as the pill and patch. Each month you put it in for three weeks then take it out for one week to get your period. After your period, you put a new one in and so on.
Effectiveness:
The vaginal ring is 99.7% effective when used correctly – worn for three weeks, taken out for one week. If not used correctly the success rate drops to 91%. You might forget to put it in after your period, it can slip out of your vagina and you have to get it back in within 3 hours and you must have it in for 3 weeks in a row. Oh dear.
What else you should know:
Some women report vaginal irritation and other similar side effects that women experience on the pill and with the patch. It may cause increased vaginal discharge, vaginal irritation, or infection as well. Ugh.
5. Birth Control Shot – Depo-Provera
Approx Cost: $20 per month or around $50 to $60 per 3-month injection
How it works:
The shot is similar to the mini-pill in that it only releases progestin in the form of depot medroxyprogesterone acetate or DMPA but unlike the mini-pill, you only have to get the shot once every 3 months. It’s mechanism essentially tricks the body into thinking it’s pregnant so an egg can’t be released.
Effectiveness:
This method is 99.8% effective if used correctly, meaning that you get the shot every 10-14 weeks. If you get it two or more weeks late, the effectiveness drops to 94%.
What else you should know:
While a shot once every three months might seem like a dream option, the Depo-Provera has a slew of side effects like significant weight gain, irregular bleeding, heavy and more frequent periods, continuous light bleeding, headaches, nausea and lower sex drive, just to name a few. As if that’s not bad enough, once you’ve taken the shot and you’re experiencing side effects, they aren’t gonna go away until the hormones leave your body in 12-16 weeks. Obviously this is not ideal.
6. Implant – Implanon or Nexplanon
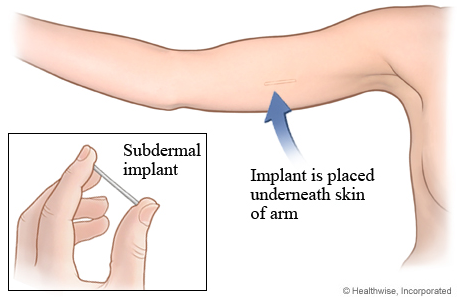
Approx Cost: $0 – $800 every three years, depending on insurance coverage and where you live. The cost for removal is $0-$300.
How it works:
Known as a Long Acting Reversible Contraceptive (LARC), the implant is a matchstick-sized rod that’s injected under the skin of the upper arm. The implant releases progestin in the form of etonogestrel (the same progestin contained in the vaginal ring) and is effective for up to 3 years
Effectiveness:
The implant is considered the most effective form of birth control next to abstinence with only 0.05% of women getting pregnant.
What else you should know:
Warning, I’m gonna have a mini rant here:
I take issue with the fact that instead of being taught how our bodies work, we we are now instead being “immunized” against our own fertility.
While this might seem like an ideal option for many women, especially teens, I urge you to think about the long-term consequences of any hormonal birth control on your physical and emotional health. There are many and hindsight is 20/20.
Additionally, if you experience side effects with the implant, you have to see a doctor and fork over a lot of cash to have it removed. See the Combined Pill section for all the side effects you might experience. The most common one I’ve seen and read about with the implant is continuous bleeding and significant changes in mood, especially depression.
Also, look at these shocking injection site images! And check out this site for user reviews and this site too – many of them are pretty awful
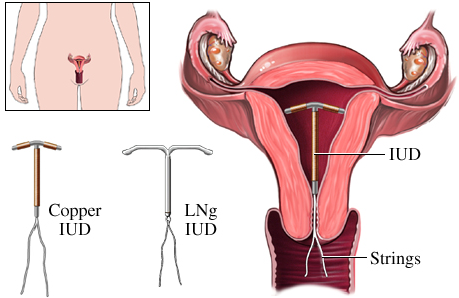
7. IUD (Intrauterine Device) – ParaGard (Copper IUD) or Mirena (Hormonal IUD)
Approx Cost: $0 to $1000 for IUD and insertion, depending on insurance coverage and where you live.
How it works:
An IUD is a small T-shaped device that is inserted into the uterus. There are 2 options for IUDs. The copper IUD (ParaGard) releases copper which is toxic to live sperm and the Mirena releases progestin to prevent ovulation. The Paragard is effective for up to 12 years and the Mirena is effective for 5 years.
Effectiveness:
The Paragard is 99.2% effective and the Mirena is 99.8% effective.
What else you should know:
While this is a long lasting option, it is expensive and there can be quite a few side effects both while you have it in and after it is removed. Women have described tremendously long and painful periods along with very heavy bleeding when using the IUD. On the other hand, many women don’t experience side effects at all. Additionally, there is the chance that the IUD can fall out and can migrate and tear uterine tissue. If this happens it may need to be surgically removed. Interestingly, IUD’s have one of the highest satisfaction and continuation rates among patients.
Barrier Methods
1. Male condom
Approx Cost: $1 each and sometimes they are available for free. I recommend L Condoms, because they don’t use glycerin or parabens and they distribute condoms in high-risk areas to people who can’t afford them. Also, Sir Richards is good for people who have latex allergies and Glyde for vegan condoms.
How it works:
A thin sheath made of latex, polyurethane, animal membrane, silicone or other material that is placed over the penis right before intercourse. You were paying attention in sex ed class right? J
Effectiveness:
When used correctly, condoms only have a 2% failure rate but that drops significantly to 18% if used incorrectly. This could include putting it on or removing it incorrectly.
What else you should know:
They’re really not that bad, especially if you’re tracking your cycle and know your fertile days. You’ll only have to use condoms for 5-7 days of the month in that case. Check out this video on how to use condoms the right way if you don’t know.
2. Diaphragm
Approx Cost: $15 – $50, and the spermicidal jellies, foams, or creams that you need to use with it range from $7 – $18 per tube
How it works:
A diaphragm is a silicone dome that you place over the cervix before sex. It works by physically blocking sperm from entering the uterus combined with spermicide that kills the sperm.
Effectiveness:
The diaphragm is not super effective. If used correctly, it prevents pregnancy 94% of the time but if used incorrectly that drops to 88%. It makes sense to combine it with a condom or the withdrawal method to increase effectiveness.
What else you should know:
While the diaphragm is inexpensive and has no adverse effects on your health (YAY), it can be difficult to insert, can move around during sex, can’t be used during your period and has to be put in right before the fun begins which is kind of a mood killer.
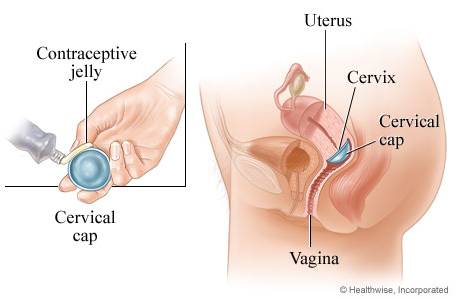
3. Cervical Cap – FemCap

Approx Cost: $89 for a FemCap kit
How it works:
The Femcap cervical cap is basically the diaphragm’s little sister. It is smaller and slips into place over the cervix and it also needs to be used with spermicide. Unlike the diaphragm, it comes in 3 sizes.
Effectiveness:
It is even less effective than the diaphragm, with only an 86% effective rate for women who have not had children and 71% for those who have.
What else you should know:
I’ve never used it and have not spoken to anyone who has, so can’t comment so much on user experience. I recommend you check out femcap.com for everything you need to know about how the FemCap works.
4. Birth Control Sponge – Today Sponge
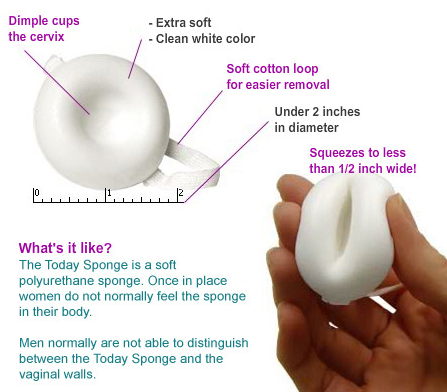
Approx Cost: $0 – $15 for a pack of 3 sponges depending on where you live and insurance coverage.
How it works:
Sold as the Today Sponge, this birth control option is made of plastic foam and contains spermicide. Like the diaphragm, it is inserted into the vagina before sex and blocks the cervix from sperm while the spermicide kills the sperm. It’s sold at pharmacies and is intended for one-time use only.
Effectiveness:
Women who have never given birth and use the sponge as directed have a 91% effective rate, while women who don’t use it as directed have an 88% efficacy. It drops significantly for women who have given birth: 80% for those who use it correctly and 76% for those who don’t.
What else you should know:
There is an increased risk of Toxic Shock Syndrome (maybe because of the plastic) and yeast infections if left in for longer than 24 hours. Some women report vaginal irritation from the spermicide. Check out: http://www.todaysponge.com/ for more deets.
Summary
Okay that’s it folks! Exhausting isn’t it? By providing this information I am not trying to overwhelm you, although the myriad options are most certainly staggering. Instead I want to invite you to get to know your body and figure out what is best for you to be at your optimum health and happiness.
Also, I know that my recommendations are somewhat biased but I cannot in good conscience recommend hormonal birth control because I just know too much! When you put synthetic hormones into your body you become another guinea pig for the pharmaceutical industry AND they win in the end with huge profits – $20 billion worldwide to be exact! With that said, you’ve gotta make the right decision for you and I respect every woman’s individual health choices. #girlpower
Most importantly, if you need guidance around coming off hormonal birth control, I’ve created the ultimate step by step protocol to help you transition off hormonal birth control (the pill (patch, IUD, implant etc) and take back control of your hormones, your body and your life. Check out my Ditch Your Birth Control Protocol here!
PS. I didn’t cover the female condom but you can learn about it here. I also didn’t mention Emergency Contraception/Morning-After pill because it is not a long-term contraceptive option. You can learn all about emergency contraception here.
References
1. http://humrep.oxfordjournals.org/content/22/5/1310.full
2. 93. Zuckerman Z, Weiss DB, Orvieto R. Does pre-ejaculatory penile secretion originating from Cowper’s gland contain sperm? J Assist Reprod Genet. 2003;20:157-9.
3. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0014812/
4. http://www.ncbi.nlm.nih.gov/pubmed/21477680
5. http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/choosing
6. http://www.plannedparenthood.org/health-info/birth-control/fertility awareness#sthash.LyPnx8YX.dpuf
7. http://www.ncbi.nlm.nih.gov/pubmed/21477680
8. http://www.thebillingsovulationmethod.org/what-is-the-billings-ovulation-method%E2%84%A2.html
9. http://www.plannedparenthood.org/health-info/birth-control
10. Image credits: Todaysponge.com, Femcap.com, Healthwise.org, Orthoevra.com


17 thoughts on “Birth Control Options 101”
Hi Nicole! I just signed up for your program and am wondering, can I try the basal thermometer method while still using my hormonal birth control? I would love to know if this would be an accurate natural reading for my body? Maybe I’m not having my periods at the my natural time, as well as many other detrimental side effects. I’ve been on birth control since I was 16 and have just now begun to hear about the effects this would have on my body in the long-term. Scary right?! Thanks for your help.
Hi Chelsea, which program did you sign up for? There is no point in taking your basal temperature while you’re still on hormonal birth control because it is preventing you from ovulating, and thus preventing your cyclical hormone changes which would trigger the temperature rise. I assume you are in the BIrth Control Protocol, and would like to come off of your hormonal BC?
If you actually read the post you’d see I say clearly that the Paragard is NOT a hormonal birth control. I’m so sorry that it wasn’t placed under a new header for all my discerning readers.
Second, the Mirena website doesn’t even state clearly how the Mirena works. The majority of women I’ve met on the Mirena have spotting or no period at all – which means no ovulation. Progestins trick the body into thinking it is pregnant – again, no ovulation. Oh, and on their website they also indicate that periods may stop – again, no ovulation.
Please don’t comment on things you don’t know about.
Nicole, I refer back to this post often as I no longer am taking hormonal birth control (after 13 years of use!). My man and I don’t plan on getting pregnant so it’s great to know what all of our options are. Definitely will be trying FAM. Thanks again–super informative post!
-Claudia
http://www.behealthyhappywhole.com
I’m so glad this information is helpful to you! Thanks for following along 🙂
Wonderful review of so many options, thank you for this! This is my journey to natural, herbal and/or energetic contraception/birth control, hoping other women share their story too! https://aartiana.wordpress.com/2010/05/26/my-6-step-herbal-contraceptivebirth-control-program/
Thank you for writing this very informative article! While I am currently trying to conceive, I had to temporarily go back on the pill to heal some cysts that had formed. I would much rather use a fertility awareness method (both whike TC and not), but I have PCOS and endometriosis so the hormones actually relieve a lot of pain for me. Also, they provide me with a regular cycle when my body does not. Do you have any recommendations for women with issues like these? Would something like FAM be useful for a person like me who does not have regular cycles and hormone imbalances?
Hey Bri! I completely understand why you’re using hormonal birth control. Pelvic pain is nothing to mess with. Unfortunately, the hormones are only masking the underlying issue so it becomes difficult for your body to heal from the inside out. I think using the fertility awareness method would be great for you. It is a little more involved for women with irregular periods but well worth the effort. I highly recommend buying the book Taking Charge of Your Fertility and reading the section on tracking irregular cycles. This will shed a lot of light on how to actually track your unique cycle. I also suggest my Fix Your Period Kickstart 28 Day Program to help get your hormones back on track with the right foods and targeted supplementation. Sending you lots of love!
I love the Paragard. I love that it is a NON-hormonal birth control and has allowed me to really learn about my own body and my true cycle. I had been on “the pill” or Nuvaring since I was 16, but last year I had the paragard inserted. The insertion (and hours after) were interesting, my friend described my symptoms as contractions (having never been pregnant, I wouldn’t know), and after that I started having really heavy periods. But instead of assuming the Paragard caused these extremely heavy periods, I noted that this may be what my real period is like. It wasn’t the Paragard giving me the heavy periods, but the hormonal birth controls kept my periods from flowing the way they should. Now, a year later, things have evened out a bit. I actually have FEWER periods a year, with a cycle that is exactly, on the dot, 6 weeks (42 days) in length, with only 5 days of bleeding–1 heavy, 1 medium, and 3 light. I can’t be happier. It took me a few months for my body to really even out and get where it needed to be, but now I love listening to my own body. I use Paragard, am building up my knowledge of FAM, and withdrawal as well as condoms when we don’t want to withdraw. But I am oh so happy with the Paragard, and I have 9 more years with it.
Hey Barbara! Thank you for sharing your endless wisdom, I so appreciate it. I’ve heard of Essure but wasn’t too familiar with the controversy surrounding it. I just read up on it and whoa! WTF. The problems I read about are outrageous. Makes me so sad 🙁
Hi Rachel, I have heard of the film but don’t recommend it on it’s own because it’s just spermicide. You must use a barrier method along with it for it to be very effective. Used alone it’s only about 74-94% effective, and it must be inserted 15 minutes before sex. AND, it is only effective for one hour. Not the best in my opinion. Hope that helps 🙂
Thanks for the amazing post Nicole! Another downside to an IUD is that you can’t do the uterine self-care massage or vaginal steams with an IUD present.
I was on the pill for years, it really messed up my gut flora. I then went to the Depo Provera shot and it made my hair fall out. I now use condoms, which work well, but I just ordered the Wink Kindara thermometer and I’m going to get serious about charting, thanks to you!
BTW, have you heard of Essure? There’s an “Essure Problems” Facebook support group. It’s so sad what these women have gone through, coil migration into the abdominal cavity, nickel allergy and extreme pain leading some to get their tubes or uterus removed.
Have you heard of vaginal contraceptive films? I was just told about them recently – apparently its a kind of dissolving spermicide? I want to try them but haven’t gone for it yet.
Right on Liz!! I’m so in love with FAM and the feeling of freedom it has created for me too. I don’t know how I was ever on BC, it seems like another life time! 😉
Let’s continue spreading the good word.
xoxo
I’m a happy FAM lover too! I was delighted you chose to list it first, “dat’s wassup!” For me, practicing the Fertility Awareness Method is FUN! The surprising feeling learning FAM gave was freedom. Freedom to know my body, know my fertility and free of a prescription. Can’t complain about that!
I tried the Depo as my very first birth control option and I hated every second! I pretty much had a light period for 3 months and I kept insisting to Planned Parenthood that there HAD to be something wrong with me, but rather than be educated about why the shot would cause that, I was brushed off. So instead of getting the second shot I opted for Ortho-Tricyclen Lo and stayed on it (or its generic cousin) for 5 years. I stopped 3 years ago when my husband and I decided to try and have a baby. We’re still trying, but I don’t think I’ll ever go back on hormonal birth control again. Not with what I’ve learned about my body in the last few years!
Hi Ryanne!
Sadly, your story is quite common.No one these days thinks it’s pertinent to inform a woman of what actually goes on inside of her body! They’re usually just pushed back on the birth control cycle. Have you taken a peek at my Fix Your Period – PMS course? I think it might help you with your fertility issues. 🙂
https://nicolejardim.com/pms