What is Adenomyosis?
Adenomyosis is a condition in which tissue similar to that of the uterine lining (the endometrium) grows into the muscular wall of the uterus, known as the myometrium.
This causes the uterine walls to thicken & become enlarged. Think of it like a thick sponge lining the uterine cavity. 🧽🩸
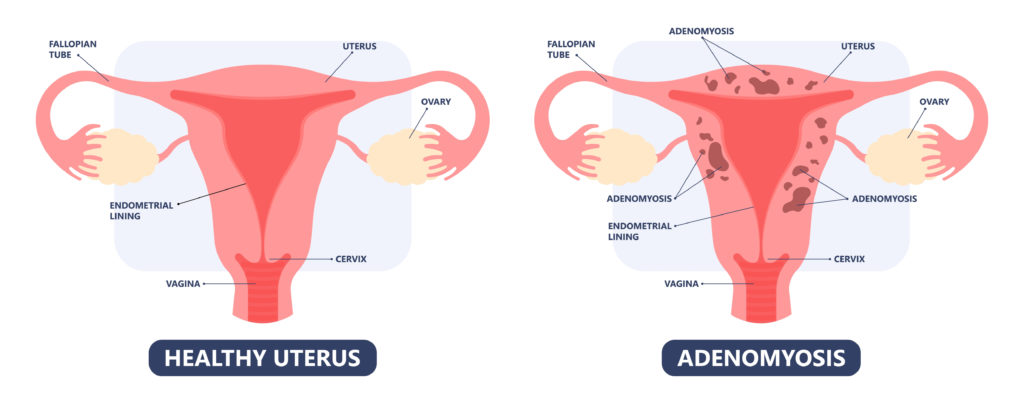
The affected tissue thickens and sheds in accordance with menstrual cycle hormone fluctuations, which leads to extremely heavy bleeding and cramping.
Adenomyosis occurs in about 20% of women with endometriosis and in about 47% of those with uterine fibroids, making for some pretty severe periods for these folks. 😣
Unfortunately, research on adenomyosis is still in its infancy and there isn’t a ton of available information about this condition.
That said, here are a few common symptoms:
- Extremely heavy bleeding that can include large clots
- Painful to very painful menstruation
- Chronic pelvic pain and painful sex
- Constantly feeling bloated in the pelvic area
- Abnormal uterine bleeding (spotting at various times in the cycle)
- Infertility (not proven to cause infertility, but infertility rates are high in women with this condition)
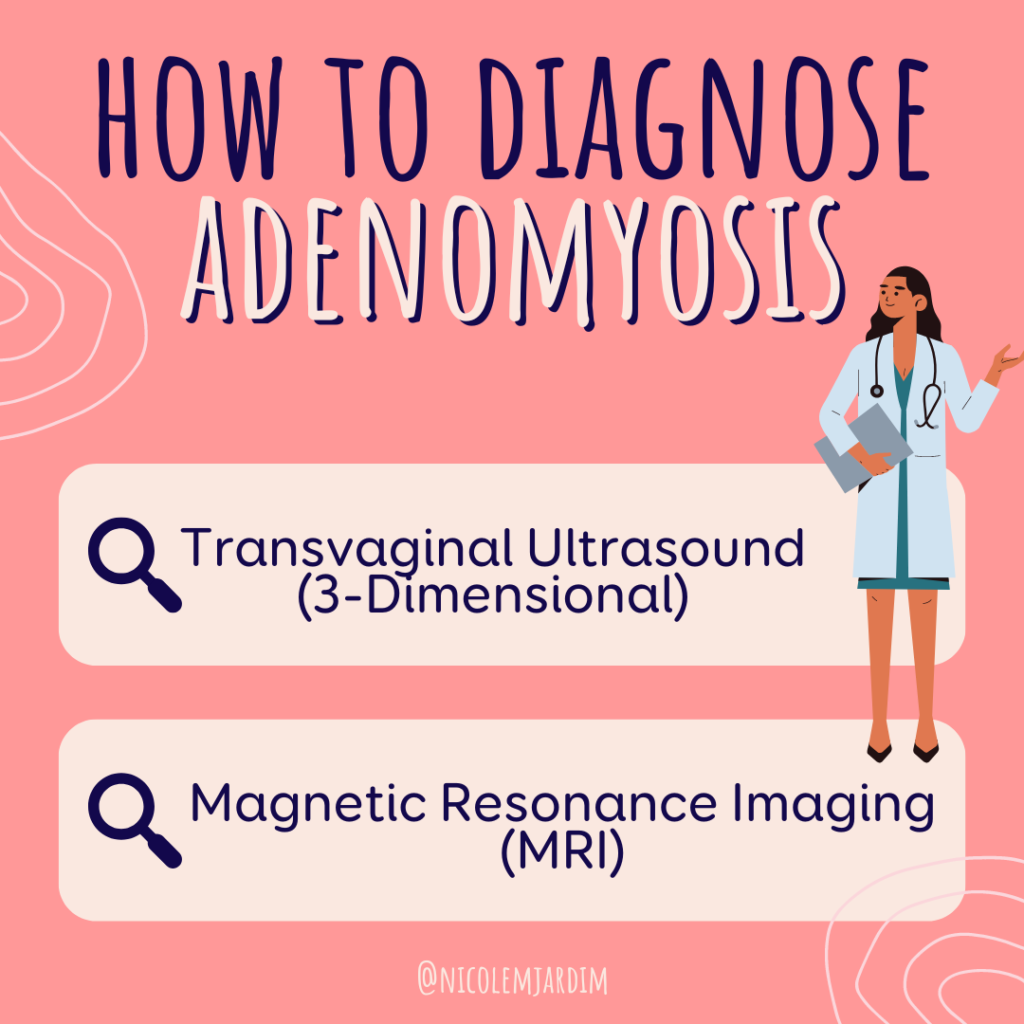
How to diagnose Adenomyosis?
Adenomyosis used to only be diagnosed via observation of the uterus after a hysterectomy…
Obviously not a very effective diagnostic tool! 🙅♀️
The first step is to rule out other causes of heavy or painful periods, like uterine fibroids, polyps, thyroid disease etc.
Nowadays, adenomyosis can be diagnosed via:
1️⃣ Transvaginal ultrasound
Studies suggest that 3-D transvaginal ultrasound is superior to the 2-D option, allowing for diagnosis at an earlier stage. Yes please! 2D creates a flat black and white image, while a 3D ultrasound consists of many 2D images taken from various angles and pieced together to form a 3-dimensional image.
All women presenting with dysmenorrhea or heavy menstrual bleeding should receive a transvaginal ultrasound to assess for adenomyosis & to exclude other structural causes (e.g., uterine polyps and fibroids).
2️⃣ MRI (Magnetic Resonance Imaging)
MRI may be used to determine the different phenotypes of adenomyosis:
- Diffuse – when the adenomyosis is distributed throughout the uterus
- Focal (also named adenomyoma)- when it affects a limited area of the uterus
Important considerations in diagnosis and treatment of Adenomyosis
If someone is asymptomatic or post-menopausal they typically don’t need treatment.
Adenomyosis disproportionately affects black women compared to women of other races. One study found black women are almost twice as likely as white women to develop adenomyosis.
It is usually diagnosed in reproductive aged women, and tends to happen later in this stage of the menstrual life cycle, usually when women are in their 30’s and early 40’s. This is all likely due to a few things:
- There is a huge lack of knowledge about this condition
- This is the time when many women are trying to conceive and might be having problems doing so
- This is also a time when many women have had one or more pregnancies which is a risk factor for adenomyosis
- Perimenopausal hormone changes are a likely driver for the symptoms associated with this condition, particularly unopposed estrogen.
🥀 The disease tends to regress post-menopause, most likely due to the cessation of ovulation and the changes in hormone production.
Causes of Adenomyosis
As I mentioned, research is lacking on this disease. That said, there are a few accepted causes of adenomyosis:
1. Women who have been pregnant and/or had an operation on their uterus are at higher risk for adenomyosis. This includes a uterine rupture during pregnancy or a surgery like a C-section.
2. Like endometriosis, adenomyosis appears to be connected to underlying immune system dysfunction.
Seems like everything is caused by that, doesn’t it?! Let’s get into it 👩🏽🔬
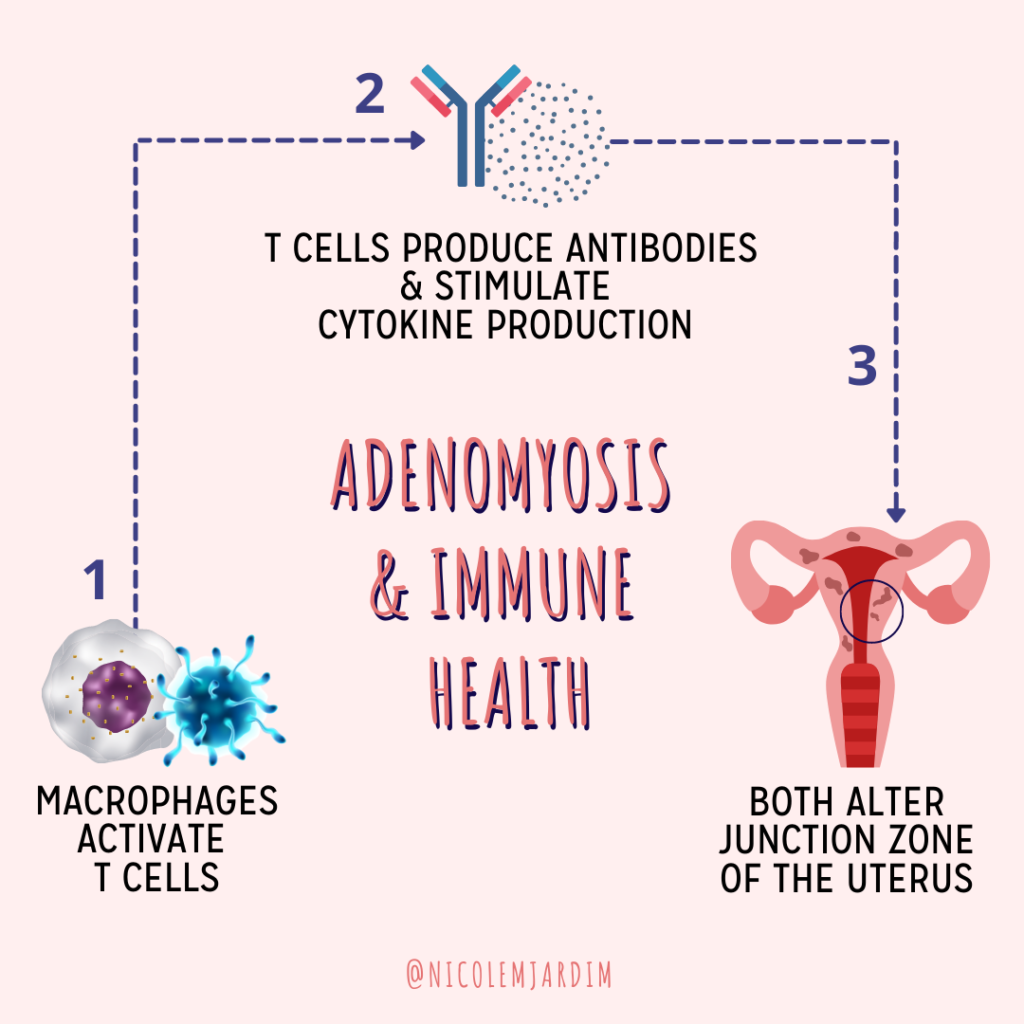
Research shows that those with adenomyosis exhibit altered immune function in the uterus where the endometrium and the myometrium meet.
A type of white blood cell called macrophages are behind this immune system abnormality.
Macrophages activate T cells ➡️ that produce antibodies & stimulate cytokine production ➡️ both of which alter the junction zone of the uterus.
The what now?!
The junction zone is the area located between the endometrium and the myometrium that changes in size due to cyclical hormonal changes.
3. The hormonal milieu likely plays a role in the initiation & growth of adenomyosis.
It appears there is a localized hyperestrogenic state in the uterus likely due to the adenomyotic tissue having a higher number of estrogen receptors + an increased response to estrogen.
Some takeaways:
1. 🚨 The tissue is invading a space that it’s not supposed to be in ➡️ which triggers a red alert from the immune system.
It’s almost identical to what happens with endometriosis.
2. As you know if you’ve been following along for a while how: It’s super important to start with gut health (I know, broken record over here – but it’s just so important!). This will do wonders for your:
- Immune response
- Blood sugar regulation
- Inflammation reduction
- Estrogen detoxification pathways (so that estrogen is leaving the body efficiently & not sticking around to feed that adenomyotic tissue)
Treatment Options for Adenomyosis
The current conventional medical treatment options for adenomyosis include:
- Pain management: Over-the-counter pain relievers such as ibuprofen and naproxen can be used to manage the pain associated with adenomyosis. Prescription pain medications may be required for severe pain.
- Hormonal therapy: Hormonal therapy aims to regulate the menstrual cycle and reduce the amount of menstrual bleeding. Hormonal therapy options include birth control pills, progestin-only therapy, gonadotropin-releasing hormone (GnRH) agonists, and intrauterine devices (IUDs) that release progestin.
- Uterine artery embolization (UAE): UAE is a minimally invasive procedure that involves blocking the blood vessels that supply the uterus with small particles. This can help reduce the amount of menstrual bleeding and relieve pain associated with adenomyosis.
- Hysterectomy: Hysterectomy is the surgical removal of the uterus and is considered the most effective treatment for adenomyosis. However, it is a major surgery and is only recommended when other treatment options have failed.
A combination of these treatment options have been found to be effective in managing the symptoms of adenomyosis. However, there are additional treatment options that I think should be front and center when working to address the symptoms associated with this condition. They include:
- An anti-inflammatory diet
- Targeted supplementation
- Natural pain reduction therapies
- Liver detoxification support to improve estrogen metabolism
- Bio-identical hormone therapy (bio-identical progesterone)
- Mental and emotional support to help navigate a chronic life-disrupting condition
Treatment options may be tailored to individual needs based on symptom severity, age, desire for future fertility, and other factors. Some examples of the alternative treatment options include:
- Diet changes: Eating a healthy, balanced diet and avoiding certain foods that can exacerbate inflammation, such as processed foods and sugar, may help reduce symptoms associated with adenomyosis.
Start with learning how to make your plate. I explain this in detail in my Harness Your Hormones Program and I’ll be giving you even more helpful eating tools in my brand new Fix Your Period Collective Membership (coming June 2023)! - Acupuncture: Acupuncture involves the insertion of small needles into specific points on the body to promote healing and relieve pain. Some studies have suggested that acupuncture may be helpful in reducing pelvic pain associated with adenomyosis.
- Herbal remedies: Certain herbs, such as turmeric, ginger, and chamomile, may have anti-inflammatory properties and may help reduce pain associated with adenomyosis.
- Stress reduction techniques: Stress can exacerbate symptoms of adenomyosis. Stress reduction techniques, such as mindfulness meditation, yoga, or deep breathing exercises, may help reduce stress and improve symptoms.
- Supplements: Certain supplements, such as omega-3 fatty acids, magnesium, and vitamin D, may help reduce inflammation and pain associated with adenomyosis. However, it is important to speak with your healthcare provider before taking any supplements, as they can interact with other medications.
You can find a supplement protocol for adenomyosis in my Fullscript Dispensary. If you have not ordered from my dispensary before, you will be prompted to create a username and password before being able to see the supplement protocol. - Bio-identical progesterone: You can find bio-identical progesterone products in my Fullscript Dispensary. Options include
- Bezwecken Progonol
- Bezwecken PG Ovals
- Quicksilver Scientific Nanoformulated Progesterone+
- Emerita Pro-Gest
Please consult with your healthcare provider and follow dosage instructions on the label.
Plus, don’t forget to grab my book Fix Your Period if you haven’t yet! Week Three is all about loving up on your GUT and it’s full of easy tips and tricks to help improve the health of your GI tract.