Written by my Spring 2018 apprentice, Susan Tessman, a Certified Women’s Health and Nutrition Coach specializing in supporting women suffering with endometriosis and other chronic pelvic pain conditions using a holistic approach.
A young woman named Emilie recently shared her painful story with me. She said “I once reported to ER on my 60th day of bleeding, in extreme pain, and had been throwing up for 2 days. The first doctor who saw me told me that my symptoms were not concerning to him, and that as far as he knew periods were sometimes irregular and painful.”
Emilie was eventually diagnosed with endometriosis, an extremely painful disease that is one of the leading causes of chronic pelvic pain in women.
Hers is just one among an incredible number of similar stories of female pain discounted and dismissed.
As a woman with endometriosis and co-existing pelvic pain conditions, I’m only too aware of how pelvic pain can often be minimized, misdiagnosed, and incorrectly treated for sometimes entire decades of a woman’s life. Women end up being shuttled through the medical system and become more hopeless over time as they are left suffering and without answers.
What are some of the reasons women’s pain is still downplayed?
#1 It’s in your head
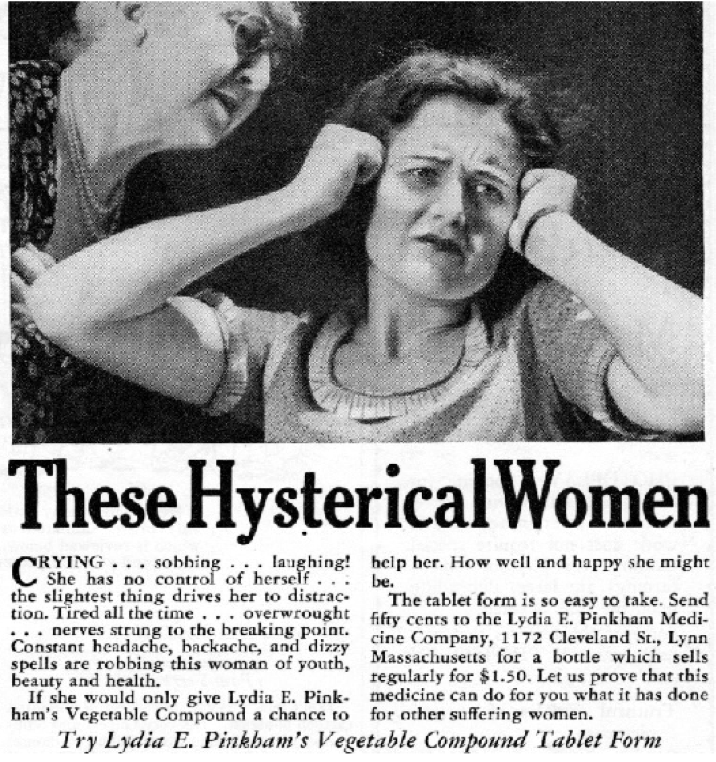
There is a long history of gynaecological disorders and pelvic pain in women being linked to mental health.
In ancient Greece, Hippocrates thought many women’s problems were caused by the uterus literally wandering throughout the body. This concept continued for centuries and because there was very little understanding of women’s biology, by the 16th century the term “Hysteria” (from the Greek word “hyster” for womb) was used to describe almost any female illness. (1)
Fast forward to the present day and a 2018 published literature review found women’s pain reports are still taken less seriously, their pain is discounted as being emotional or not real, and they receive less effective medication than men. (2)
Olivia, another endometriosis sufferer, describes her trip to the ER for extreme pain:
“A nurse at one hospital pulled my mom outside the room and said ‘It’s bizarre how she’s crying and dry heaving. I think she needs psychological help. I want her discharged immediately.”
#2 We don’t like to talk about it
Women and even practitioners are often uncomfortable with discussing female pain.
The National Vulvodynia Association found in a survey conducted in 2000 that fewer than 2.5% of women reported feeling comfortable disclosing vulvodynia (chronic vulvar pain without an identifiable cause) to their closest female friends. (3)
This discomfort can create a world of isolation for pelvic pain sufferers.
#3 Lack of research and training
Health practitioners don’t receive enough training in diagnosing and treating women’s pelvic pain conditions and because symptoms can overlap they may often misdiagnose these conditions.
Forty per cent of women with chronic vulvar pain remain undiagnosed after three medical consultations. Fifty per cent of women with endometriosis see at least five health care professionals before receiving a diagnosis and/or referral. (4)
#4 Female pain is considered normal
“When all you know is pain, you don’t know that that is not normal. It is not a woman’s lot to suffer, even if we’ve been raised that way,” Susan Sarandon
How many of you were ever told that super painful periods just ran in the family and you’d have to live with it?
A 2001 study published in the Journal of Law, Medicine & Ethics found that doctors often incorrectly believe that women have a “natural capacity to endure pain” and possess more coping mechanisms thanks to the stresses of childbirth. (5)
So the important question is how do you tell the difference between normal period pain and what could be caused by a pelvic pain condition?
>>Normal period pain
Although there is a spectrum of symptoms women will experience with their periods, if your body is in balance, normal period symptoms would be:
- pain during the first few hours to few days of your period
- mild to moderate cramping and heaviness in the pelvic area caused by uterine contractions
- some may also have mild lower back pain or loose bowels
- simple treatments like over the counter pain medications, hot water bottles or mild exercise relieve the pain
- you can continue to do your normal activities
Some women will also have twinging pain for a short time during ovulation.
>>Abnormal Pain
You may be getting pain from an underlying condition if you experience any of the symptoms below either with your period or at any other times, and on a repeated basis. The pain can interfere with your life on many levels:
- painful bowel movements
- painful bladder or urinary urgency and frequency
- pain with sex or pelvic exam
- burning and irritated vulva
- painful bloating
- severe cramping
- chronically heavy periods
- radiating pain to lower back and down legs
- pain severe enough to cause nausea and vomiting
The journey to healing from pelvic pain
One of the biggest lessons I have learned in my own journey and from working with women in pain is that we have to take charge of our healthcare and become our own advocates.
What are some of the ways you can support getting more effective results when pursuing treatment for pelvic pain?
- Find a practitioner that validates your experience, supports your specific needs and is open to your questions and ideas. Don’t be afraid to ask for second opinions.
- Keep a symptom/pain journal throughout the month, to help document your pain and connect the dots to any possible triggers.
- Make sure your practitioners are taking a detailed history of your reproductive health and physical symptoms and are open to referring you to a specialist.
- Research from credible sources and become well educated about your condition.
- Work with people who specialize in women’s pain.
Pelvic pain usually requires an approach that combines treatments. This can include surgeons specializing in excision surgery for endometriosis, gynaecologists and urogynecologists, pain management specialists, pelvic floor physical therapists, nutrition & health coaches with a focus on female pain, mind/body practice and other bodywork therapies such as acupuncture, visceral manipulation & massage, to name a few.
It’s in our power to keep the discussion of female pain open, so that cultural holdovers of shaming or gender bias don’t cause unnecessary suffering because of lost access to timely and effective treatments.
For a list of resources on pelvic pain conditions please visit www.susantessman.com/resources/
References:
- https://en.wikipedia.org/wiki/Female_hysteria
- Anke Samulowitz, Ida Gremyr, Erik Eriksson, and Gunnel Hensing, “Brave Men” and “Emotional Women”: A Theory-Guided Literature Review on Gender Bias in Health Care and Gendered Norms towards Patients with Chronic Pain, Pain Research and Management, Volume 2018, Article ID 6358624
- The National Vulvodynia Association. National Vulvodynia Association survey. 2000
- Mary Lou Ballweg & Carol Drury, Terrie Cowley, K. Kim McCleary and Christin Veasley, Chronic Pain in Women: Neglect, Dismissal and Discrimination, May 2010, Produced by endwomenspain.org
- Diane E. Hoffmann, Anita J. Tarzian, The Girl Who Cried Pain: A Bias Against Women in the Treatment of Pain, Journal of Law, Medicine & Ethics, Vol. 29, pp. 13-27, 2001
- Briden, Lara. Period Repair Manual: Natural Treatment for Better Hormones and Better Periods
- https://www.dailymail.co.uk/femail/article-3046571/How-normal-period-pain-90-cent-women-experience-cramps-month-vomiting-leg-pain-painful-sex-signs-serious.html
- Camran Nezhat, M.D., Farr Nezhat, M.D. and Ceana Nezhat, M.D, Endometriosis: ancient disease, ancient treatments, Fertility and Sterility, 2012. American Society for Reproductive Medicine.
About Susan:
For more resources on support for endometriosis and pelvic pain please visit www.susantessman.com