Written by my Fall 2020 Apprenticeship Participant, Alexandra Mayer. Interested in joining my next Apprenticeship? Sign up for the waitlist here.
Becoming a mother is magical – nine months of waiting and anticipation, the kicks and turns of the baby, and, of course, the day your little bundle of joy is born. When I became pregnant my knowledge of what to expect from pregnancy wasn’t very extensive, but I had a good idea of what would happen to my body, for how long, and what would happen at the end.
As I moved forward, week to week, everything was preparing me for the “Day X”-books, courses, moms’ groups, I even easily found a video of an actual birth online! So when my due date came, I was so ready. And it was magical indeed!
What I didn’t know and wasn’t prepared for was what would happen after a few weeks, a few months, and even a few years (yes, hormones can fluctuate and influence you for even 1-2 years after the birth).
- What happens now?
- Why hasn’t my period returned yet?
- Do I need to and how to track my cycle if I don’t have a period?
- My baby is almost 1 now, so why is my hair still falling out and why do I feel so sluggish?
Despite being a hormonal health nerd and knowing a lot about menstrual cycles I didn’t have all the answers. I’ve spent hours and hours on research to answer these and many other questions, and found so much controversial and at times conflicting information.
Postpartum is a long period and has its milestones, that is why to keep it clear all the information is divided into a few sections based on the period of time after the birth.
The first 6 weeks
The postpartum period begins right after you give birth, and its first phase lasts about 6 weeks. Here’s what to expect during this time:
Bleeding
One of the most prominent symptoms you will experience is the vaginal discharge called lochia. It lasts for about 4-6 weeks and consists of tissue, uterine lining, mucus, and blood that were produced by your body during the pregnancy. That is why lochia occurs after both natural births and C-sections.
It most likely will feel like your period, but it may be heavier and lasts much longer. Lochia usually starts bright red and slowly transforms to a pinkish-brownish, yellowish-whitish, and eventually a transparent discharge. It often comes with cramping, because during this time your uterus continues to shrink to its normal size.
Definite warning signs and reasons to call your doctor are abdominal pain and/or swelling, ongoing bright red bleeding, large clots, fever, or an unpleasant odour. Those might indicate residual tissue in the uterus that needs to be removed.
Also, a very light or short bleeding is a reason to talk to your midwife or doctor because your uterus might need some support in shrinking and expelling tissue.
Hormones
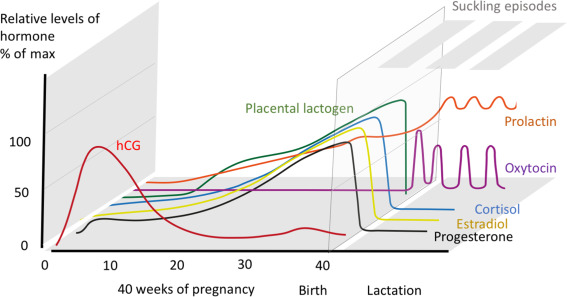
The birth causes probably the most powerful change possible in women’s hormones. During the pregnancy the main female hormones, such as progesterone and estradiol, significantly rise from around week 30 until the birth that marks a strong and abrupt drop in those hormones.
This drop is associated with various psychological symptoms such as mood swings, anxiety, and even depression.
Postpartum depression is a real thing; according to the NHS (1), 1 in 10 women will develop associated symptoms within the first 12 months after giving birth.
This is a very important topic that deserves a separate post; you can read more about this topic here.
Please do not ignore your “baby blues” or listen to those who say you are just tired. If your mood is persistently low and includes signs of sadness or depression, please seek help.
The hormone levels will stay on the low side until your body is ready to reproduce again and your fertility returns.
In case you decide to breastfeed, there are 2 more important hormones you should know about: prolactin, which is the star of milk production and oxytocin, the “cuddling” or “feel good” hormone.
You know that feeling when you hold your little one and get a tingling sensation in your breasts and feel milk flushes? Oxytocin is responsible for that. These two hormones are also responsible for ovulation suppression (2) and will most likely be your companions until you reduce the number of feedings or wean your baby completely.
The doctors’ check
Another important thing that happens at the 6-week milestone is a checkup by your ob-gyn. The doctor will check the size and condition of your uterus, cervix, healing of the abdominal scar in case you had a C-section, and healing of birth injuries and scars if you had any.
Also, your doctor should check (or direct you to someone who can) whether you have a diastasis recti (a muscle separation along your belly midline) and whether you have a prolapse of your pelvic organs.
If everything is fine at this appointment your doctor will also clear you for sexual activity and sports. For some women, 6 weeks is a good time to return to those activities, for others, however, it might take longer. The most important thing here is to listen to your body, and give it as much time as it needs.
Dos and don’ts
The first weeks after the birth are absolutely crucial in the process of healing, and I believe these steps are essential. Small daily things we do can have a huge impact.
- Rest, Rest, Rest. The first 6 weeks postpartum are called “Wochenbett” in German, which literally means “weeks of bed”, and this makes so much sense. Resting and lying down are crucial at this time. The organs that were squeezed by the baby for months need time to adjust and reposition. Gravity is no help here.
- Standing Up. Whenever you have to stand up (only if you absolutely need it; remember the Rest, Rest, Rest point) do not just pull your torso upward. Instead, turn to the side and then stand up from there. This way you will prevent your rectus abdominis (that “six pack”) muscle from contracting and help heal diastasis recti.
- Sneezing. Another tip to help diastasis recti and the recovery of your pelvic floor is to adjust the way you sneeze. Sneezing creates a huge intra-abdominal pressure and thus makes your abdomen and pelvic floor muscles stretch, which is not advisable in the first weeks postpartum. Turning your head towards your shoulder before sneezing reduces the pressure and makes sneezing less harsh on your abdomen and pelvic floor.
- Crossed-Legs Position. This one was the hardest change but made me start feeling my pelvic floor again. Sitting in a crossed-legs position (like you would traditionally during meditation) stretches your pelvic floor muscles, which is even beneficial under normal circumstances. However, after carrying quite some weight during the months of pregnancy, and in case you pushed the baby out during a natural birth, the last thing our pelvic floor needs is a stretch.
- Exercise. Do not rush. Please, please, please give your body time to heal! You will have so much time and energy to get back in shape – just a little later! We live in a world where, unfortunately, very often new moms are concerned about “bouncing back” quickly instead of celebrating motherhood, themselves, and their bodies for making the miracle of a new life. However your body looks now, it’s beautiful! Healing and your baby are now your priorities; everything else can wait. Moreover, proper healing will ensure that when you’re ready and want to, you’ll get back in shape much faster and easier. When you are cleared by your doctor and actually feel like it again, start slowly. I always recommend special postpartum courses and Pilates before any other type of workout. With such a start you’ll gain back the strength from within, reactivate the deepest muscles that were weakened during the pregnancy and birth, and prepare your body for any harder exercises and activities.
Weeks 8-12 and beyond
By this time, you’ll probably be a little bit more settled and used to your new lifestyle and role of mom. This milestone, however, can bring some new symptoms and questions.
Hair loss
Almost every woman sees postpartum hair loss. Around the 3-6 month mark, you might notice more hair in your brush. This is caused by the drop of estrogen after the birth and can last for a few months, so there’s no need to panic; it’s rather normal and will most likely get back to normal by your baby’s first birthday.
Excessive shedding, though, along with feeling sluggish and tired all the time, might be signs of iron deficiency, or postpartum thyroiditis that occurs in around 8% of women post-pregnancy (3).
So if you are unsure or your symptoms prevail for longer than a year contact your doctor and ask to check your thyroid. Also, make sure you’re eating enough, your meals are nutrient rich, and you have good pre/post-natal supplements. Nicole has a great list of those worth attention on her period portal.
Return of fertility
Another big question is “when will my fertility return?” I think I’ve spent the most time researching this one, and the most common answer is “it depends.” If you decide against breastfeeding your fertility may return shortly after your lochia stops around week 6 postpartum. On average, a nonlactating woman will ovulate with a consequent period somewhere between 45-95 days postpartum (4).
It gets a bit more complicated with breastfeeding. As we already know, the hormones prolactin and oxytocin that ensure lactation are also responsible for ovulation suppression.
The lack of ovulation and periods while breastfeeding is called Lactational Amenorrhea and, under certain conditions, can even be used as a method of birth control with a pregnancy chance of only 2% (5).
Some women will resume cycling faster than others. According to Natural Child Spacing and Breastfeeding by Jen O’Quinn, around 7% of lactating women will resume cycling 0–6 months postpartum, 37% between 6 and 12 months, and 48% between 12 and 24 months; 8% will experience suppressed fertility longer than that.
Your fertility might return as you reduce the number and duration of feedings, especially at night when prolactin levels are higher (6). However, some women will start ovulating again only after weaning the baby completely. This is, however, a good thing that is called natural child spacing and ensures your body has fully recovered and is ready to have a new healthy pregnancy.
Your cycles and periods might also be irregular at first and different from what you had before pregnancy. Give it some time, as your hormones balance out, your cycles will regulate, and your “new normal” will establish.
Postpartum cycle charting
There are many myths and concerns around postpartum cycle charting out there, which discourages many mothers from even trying. The truth is, cycle tracking and Fertility Awareness Method (FAM) are definitely manageable and have been practiced successfully by many postpartum mothers.
If you have used FAM before and are familiar with fertility signs, it will probably be easier for you. The way to chart and the rules may vary depending on the method; however there are basics that are common:
- Temperature is not an essential tool until fertility actually returns. Temperature has no predicting value; therefore, it won’t help you detect the signs of returning fertility. Sleepless nights might also be a challenge for temperature tracking. You can start taking your temperature when you notice you are in a fertile window to confirm ovulation. Some wearable devices such as Tempdrop or Trackle measure your temperature during the whole night and can be a good option for moms who wake up frequently to take care of the baby.
- Cervical fluid is the main sign you should look for. Start observing your fluid after lochia stops. First, you’ll need to establish your basic infertile pattern to make sure you will notice when the transition to fertility happens. Track your fluid for 2–3 weeks and see what is typical for you. Most of the time it will be no mucus at all (dry days) or some whitish, creamy mucus. After you know your infertile pattern it will be possible for you to notice a change in it as you reach your fertile window- cervical mucus will become transparent, stretchy, like egg whites.
- Even if you’re an experienced charter, postpartum charting can get tricky; therefore, working with an instructor at this stage is beneficial and helpful. Lisa Hendrickson Jack’s Fertility Friday offers a lot of information, podcasts, and even courses on postpartum charting and is a great place to start.
Post-weaning
This stage is probably the one least talked about. Weaning, however, causes quite a big hormonal change and might introduce new symptoms.
- Psychological symptoms. Remember that “feel good” oxytocin hormone? It also helps you to deal with sleepless nights better. So stopping breastfeeding will reduce levels of oxytocin, and having disrupted night sleep might hit you hard by causing irritability and fatigue.
- Weight gain. The hormone prolactin is known to affect fat metabolism and promote fat storage (7). After weaning it takes a while for the prolactin level to decrease, and in combination with the loss of those 500–700 calories burned by breastfeeding, slight weight gain might happen.
- Changes in skin. You might also experience some acne and breakouts during this time as a result of the initial estrogen and progesterone imbalance.
- Estrogen rising. Weaning also has a bright side. As estrogen increases, you might notice that your mood improves and your libido finally appears.
You can make this transition easier for yourself by taking it slow, gradually reducing feedings. A nutritious diet with lots of vegetables, lean proteins, healthy fats, and micronutrients; regular exercise and self-care will help your body to regulate hormones easier and faster.
Also, don’t underestimate the psychological stress weaning can cause you and your baby. Spending lots of time with the baby, cuddling, playing, and enjoying each other’s company will soften this important step for both of you.
Postpartum is definitely a process and has its ups and downs. Yet the joy of motherhood and the loving little human being who will call you mom very soon are totally worth it. So enjoy it and embrace whatever it brings.
Sources
1. https://www.nhs.uk/mental-health/conditions/post-natal-depression/overview/
2. P W Howie, Breastfeeding: a natural method for child spacing, American Journal of Obstetrics and Gynecology, Volume 165, Issue 6, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4989649
5. https://www.llli.org/breastfeeding-info/birth-control/
About Alexandra

Alexandra is a holistic Pilates trainer and a women’s health enthusiast based in Munich, Germany. By recently graduating from Nicole Jardim’s Fix Your Period Apprenticeship Program she is pursuing her passion and a dream to open up the fascinating world of healthy hormones to Russian speaking women, to help them understand their bodies, live in harmony with their cycles and embrace femininity in every aspect of their lives. You can connect with Alexandra on her Instagram @the.fem.muse.