I get so many questions about IUDs (hormonal intrauterine devices), which is understandable considering the fact that they seem like the prom queen of birth control these days.
Women are frequently sold on the convenience of not having to remember to take a pill on the daily to prevent unwanted pregnancy (totally get it!). And, they’re drawn into the promises from their doctors of not having a period and not having to think about getting pregnant for at least a few years. (Also get that too!).
But, you know, when something sounds too good to be true, it might be, right?
While hormonal IUDs can absolutely be a blessing for many women (I don’t want to discount that), they are not without side effects to our body’s natural hormones.
And while so many of us dream of not having to think about birth control or deal with our period problems anymore, not having a period is actually not a great thing. Our bodies were designed to ovulate. While you might have been told otherwise, these hormonal IUDs can (and often do) prevent ovulation.
What we really should aspire to is addressing our period problems from a root cause perspective so that we can reduce our symptoms to manageable levels.
You can start understanding why you’re having symptoms by taking my free period quiz.
How Does The Mirena IUD Work?
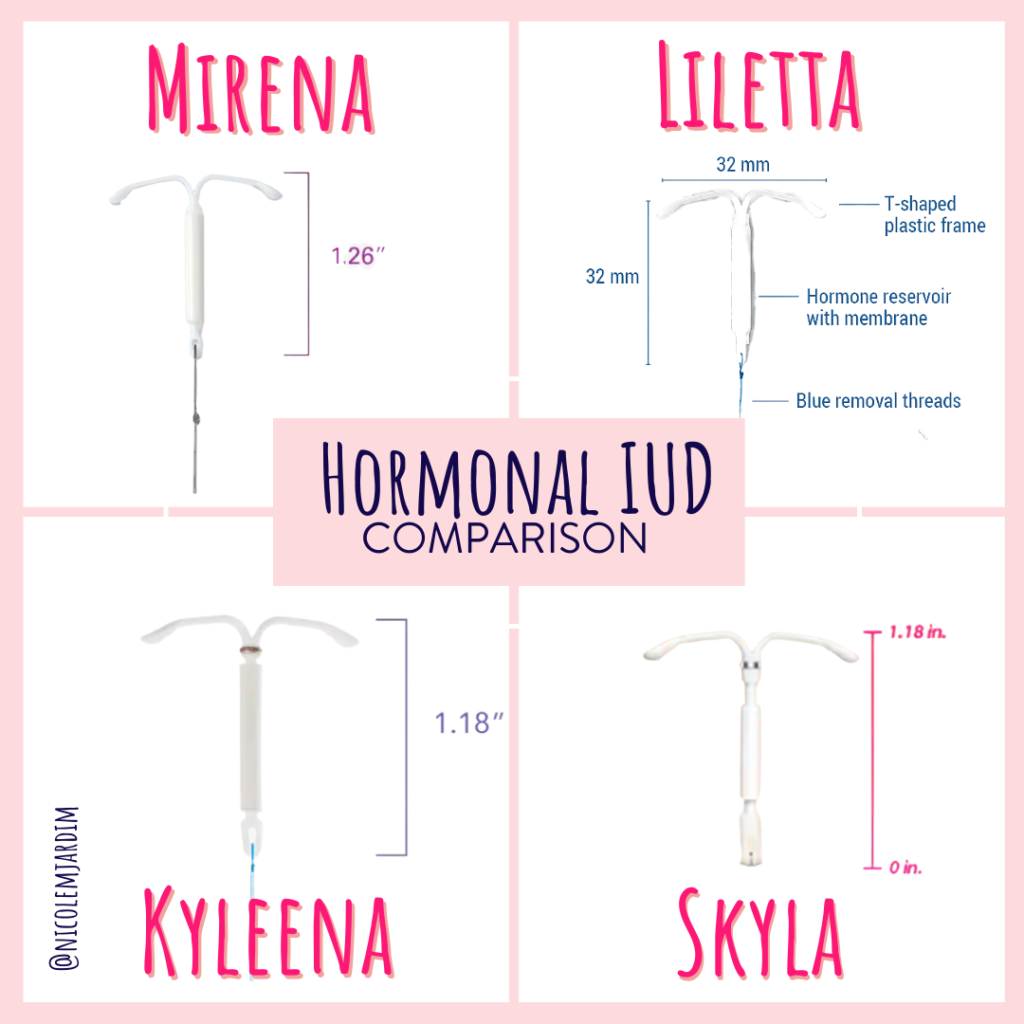
An IUD is a “T” shaped device that is inserted into the uterus via the cervix in an outpatient medical procedure.
Hormonal IUDs are known by several brand names in the US, including:
- Mirena®
- Kyleena®
- Liletta®
- Skyla®
Just to clarify, there are also copper IUDs that are used as a form of birth control, but they don’t emit hormones the way these hormonal IUDs do. Same idea, different execution.
According to the folks who manufacture the copper IUD, it works by preventing sperm from reaching the egg. In a nutshell, it prevents pregnancy by creating an inflammatory response in the uterus which inhibits implantation. Additionally, copper is also toxic to sperm.
So how do hormonal IUDs prevent pregnancy?
They release progestin into your body, which is a synthetic version of the hormone progesterone.
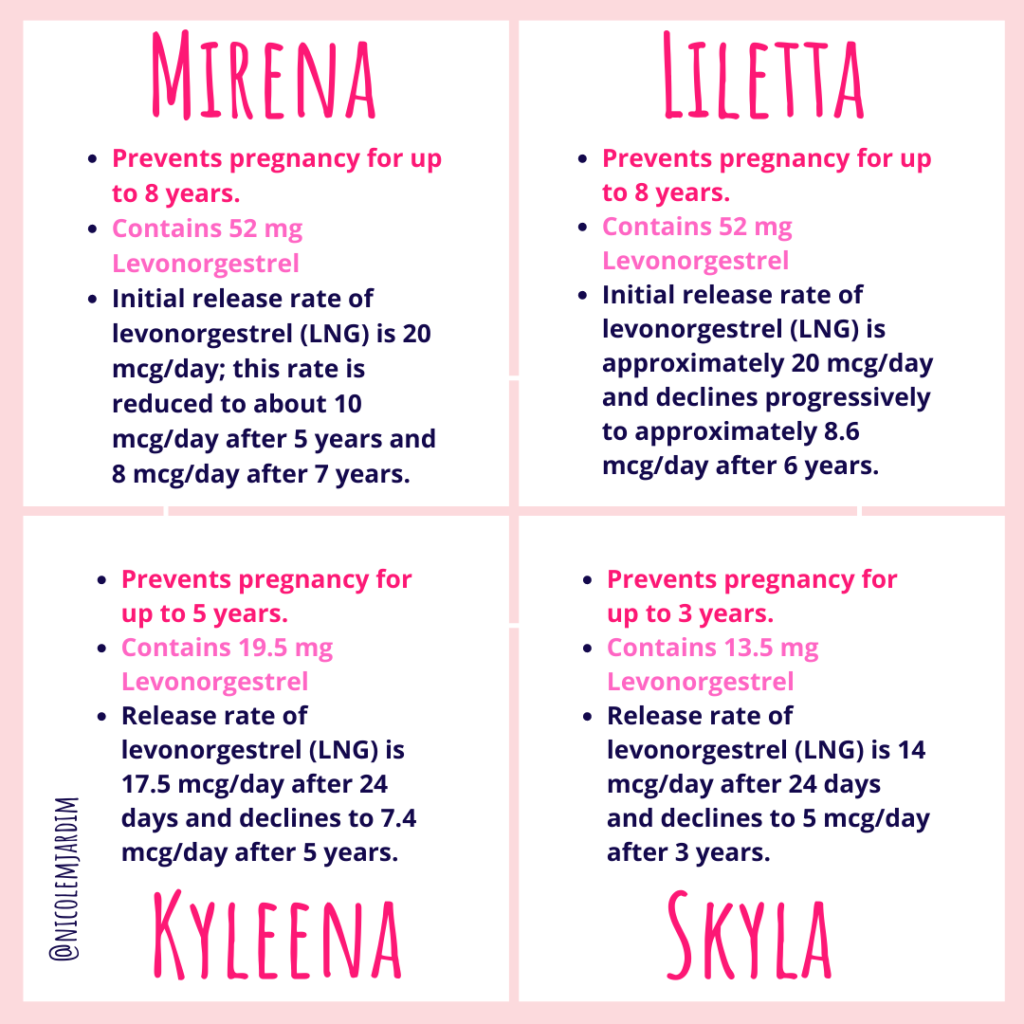
Each IUD contains 13-52 mg of the progestin known as Levonorgestrel (LNG). Over time, they release a tiny bit of this hormone into your body Every. Single. Day. Between 8-20 mcg of the drug are released daily over the lifespan of the IUD. And depending on the brand of IUD (see brand names above), it can last between 3 and 8 years.
This progestin prevents pregnancy in a few ways:
First, it thins the uterine lining out so much that implantation of a fertilized egg becomes impossible. This is actually part of the reason why someone would have lighter periods or why their period would disappear completely while on a hormonal IUD.
Progestin can also thicken cervical fluid, which makes it more difficult for sperm to reach an egg.
Does The Hormonal IUD Prevent Ovulation?
According to the FDA label, and the Mirena® package insert, hormonal IUDs can prevent a woman from ovulating, especially in the first year of use. After the hormones the IUD releases start to wane, ovulation can return for all but 25% of users.
On the other hand, with brands of different IUDs like Skyla® (lower progestin levels), ovulation doesn’t appear to be affected much. Other studies estimate that ovulation is affected in 5-15% of women, and seems to correlate to the amount of Levonorgestrel that the IUD is secreting.
While their primary mechanism of action is to thin out the uterine lining and thicken cervical fluid, hormonal IUDs definitely interfere with ovulation and your regular menstrual cycle, so there’s bound to be a few changes after you’ve had one placed. In my experience, the majority of women on the Mirena IUD I’ve worked with stop ovulating and/or lose their periods which appears to go against what the studies say.
Hey, when you’re working with human bodies, there are a lot of variables!
Check out the package inserts for the four different current types of available IUDs, so that you can make a fully informed decision before going on a hormonal IUD:
What Are The Advantages Of Hormonal IUDs?
You didn’t think I’d tell you all the bad things and not give you the pros of using a hormonal IUD right?
IUDs can be easier to insert if you’ve had a baby, since the cervix is a bit more lax in women who’ve given birth, but even if you haven’t had a child, an IUD can still be inserted, so pretty much any woman can utilize them.
Hormonal IUDs like Mirena offer long term birth control and you don’t have to remember to take a pill every day, or continually change a patch or vaginal ring.
Additionally, the Mirena is often placed to help reduce heavy periods (because the progestin thins the uterine lining).
If you have heavy and long periods, definitely take my Period Quiz to find out what could be going on with you.
And while all of this can be a very attractive solution for many women, it raises the question — why should we have a foreign object in our body every single day when we only need to protect against pregnancy for a few days every month?
ICYMI: there are more natural birth control options that don’t involve having a piece of plastic emit hormones into your body every day for 5 years.
What Are The Possible Side Effects Of The Mirena IUD?
This of course brings me to the side effects of the hormonal IUD, which are very similar to the side effects of oral contraceptive pills. When the hormonal IUD is first inserted, many women report an extremely painful experience. Cramping and bleeding can be severe for the first several months after the IUD is placed in some women, and in others their period disappears completely.
Some of these common side effects may include:
- Headaches
- Pelvic pain (if ongoing, it could be a sign of IUD perforation)
- Back pain or tailbone pain
- Long, heavy periods after it’s first inserted for some women
- Irregular bleeding and spotting
- Loss of period (amenorrhea) for others
- Vaginal microbiome disruption which causes yeast infections and bacterial vaginosis
- Breast tenderness
- Depression or a depressed mood
- Stomach problems like bloating, gas, diarrhea and constipation
- Weight gain (sometimes severe)
- Ovulation disruption which reduces your sex hormones estradiol and progesterone. This can lower sex drive and cause vaginal dryness
- Acne
Sometimes, women experience rare, serious side effects from hormonal IUDs.
These may include:
- Blood clots
- Migraines
- Stroke
- Allergic reaction to the IUD
- Increased blood pressure
- Ectopic pregnancy
- Pseudotumor Cerebri (a brain tumor mimic caused by pressure in the brain)
Other complications can arise if the uterus is perforated by the IUD. This can happen in rare instances, about 1 in 1000 insertions. If the IUD “wanders” it can move outside of the uterus, possibly causing infection and scarring. Surgery may be required to have the IUD removed if this happens. If your IUD has wandered, you will likely experience pelvic pain that doesn’t subside or not be able to find the IUD strings.
Pelvic Inflammatory Disease (PID) is another concern. Usually, PID is caused by gonorrhea or chlamydia. However, as stated on the Mirena package insert, PID is a serious infection that is considered a potential side effect of the IUD. If you currently have PID, it is not recommended to have an IUD inserted, as it could lead to the spread of the infection. Also, please make sure that you are screened for any sexually transmitted infections before having an IUD placed.
I’d love to hear from you. Did your doctor explain these potential side effects to you? If not, can we agree that we deserve more and better treatment from the traditional medical establishment?
What Do I Do If My IUD Is Expelled?
If your uterus decides to expel your IUD, it’s not really as scary as it may seem. Be sure to call your doctor right away and have it looked at. This goes without saying, but please don’t try to put it back in yourself.
Be sure to check often that you can feel the strings of the IUD to make sure it’s in place. And if at any time, you’re afraid your IUD is missing or if you’re experiencing any of the following, call your doc right away:
- Fever
- Heavy bleeding
- Pain
- Cramping
No Ovulation Is No Bueno
So, we’ve talked about how the hormonal IUD works by thinning the uterine lining, thickening cervical fluid and sometimes by preventing ovulation.
Here’s the thing — we are supposed to ovulate. Can I shout this from a rooftop?! Our bodies were designed to have pain-free, symptom-free monthly cycles where an egg is released, and then the lining of our uterus is either shed or we get pregnant.
Stopping ovulation from occurring is not only stopping the natural function our reproductive system is supposed to carry out, but it’s also jeopardizing our overall health.
When we don’t ovulate, progesterone isn’t produced, and this hormone is key in so many of our bodily functions. Progesterone in the right amounts prevents estrogen levels from climbing too high, so when there is not enough of it we get more crazy PMS, super sore boobs, heavier periods, an increased likelihood of certain cancers, and bone loss.
What’s more — having this kind of IUD can mask some pretty serious conditions, like polycystic ovary syndrome (PCOS), thyroid problems, or even pituitary tumors (which stop ovulation and make your period disappear).
When we prevent ovulation, we’re unnecessarily suppressing the normal function of the human female body. It’s important for me to reiterate that stopping ovulation is certainly not the only way to prevent pregnancy. I’d recommend checking out the Fertility Awareness Method and other cycle tracking options like the devices listed in this post as alternatives.
Take a listen to my Period Party Podcast episode “What’s A Period And Why Do I Need One?” To learn more about your cycle and the important benefits of ovulation.
What to do next?
Look, I’m all for women having access to all of the birth control they can possibly get their hands on.
But what I’m really in favor of is education — about the true nature of hormonal contraception and the side effects it can have on our health.
Traditional medicine is not talking about these side effects and the long-term ramifications for women and the planet.
So — if you love all things hormones, female health, and learning about everything your doc should discuss with you but doesn’t…we should be friends! You shouldn’t have to be a medical professional to understand how your body works and what to do to take care of it properly.
Start with my in-depth Period Quiz to start getting real answers about your period and hormones.

Sources
“Mirena (hormonal IUD) – Mayo Clinic.” 5 Sep. 2019, https://www.mayoclinic.org/tests-procedures/mirena/about/pac-20391354.
Historical record-setting trends in IUD use in the United States.
https://www.ncbi.nlm.nih.gov/pubmed/29842865
“Mirena® (levonorgestrel-releasing intrauterine system … – FDA.” https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/021225s019lbl.pdf.
“Mirena – Bayer.” https://labeling.bayerhealthcare.com/html/products/pi/Mirena_PI.pdf.
“Reference ID: 3242566 – FDA.” https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/203159s000lbl.pdf.
“Pharmacokinetic and pharmacodynamic studies of … – NCBI.” https://www.ncbi.nlm.nih.gov/pubmed/2335100.
“Safety, efficacy and patient acceptability of the … – NCBI.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2971715/.
“Role of the levonorgestrel intrauterine system in … – NCBI.” 9 Aug. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3749061/.
“Progestin (Oral Route, Parenteral Route, Vaginal Route ….” 1 Sep. 2019, https://www.mayoclinic.org/drugs-supplements/progestin-oral-route-parenteral-route-vaginal-route/description/drg-20069443.
“Management of pain associated with the insertion of … – NCBI.” 12 May. 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3682672/.
“Intrauterine devices and risk of uterine perforation – NCBI.” 16 Mar. 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5683155/.
https://www.ncbi.nlm.nih.gov/pubmed/7984332.
Levonorgestrel intrauterine system (Mirena): An emerging tool for conservative treatment of abnormal uterine bleeding
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4389381
“Intrauterine devices & infection: Review of the … – NCBI – NIH.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4345753/.
“Migraine with aura increases the risk of stroke – NCBI.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4540227/.
“Hormonal contraceptives and risk of ischemic stroke in … – NCBI.” 30 Oct. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5662520/.
“Estrogen Dependent Cancers – Cleveland Clinic.” 22 Aug. 2013, https://my.clevelandclinic.org/health/diseases/10312-estrogen-dependent-cancers.
“Progesterone & Bone Health – Women in Balance Institute.” https://womeninbalance.org/resources-research/progesterone-bone-health/.

4 thoughts on “How Does the Mirena IUD Work? Is it Right For Me?”
I would love your take on partial hysterectomy. I really like my Mirena, but I definitely still ovulate. I think I also have a sort of sub-clinical PCOS (soaringly high hormone levels), so I am really concentrating on controlling my blood sugar. But i feel like the Mirena is contributing to cysts – normal follicular and luteal ones, but they must be large because I can feel them as they change and they can hurt. Plus my uterus is retroverted and moving even further backwards and to the side (which incidentally resulted in my first Mirena being inserted into my uterine lining by a lazy midwife who thought that level of pain was normal….but the next one under ultrasound didn’t feel like anything). I kind of want my uterus gone so I don’t need an IUD and it stops laying on my poor colon. It’s a scary idea though, and not something I’ve broached with my doctor. Just been thinking my insides could use less literal pressure pushing on them.
Hi there! I can’t give you medical advice so you’ll have to speak with your doctor about all of this. However, your tilted uterus is tilted for a reason. Please consider finding a pelvic physical therapist or visit my friend Barbara Loomis’ website https://alignmentmonkey.nurturance.net/ to learn more about why your uterus is not in the right position. Additionally, it is important to work one on one with a certified women’s health coach, nutritional therapist or registered dietician who can help you figure out the right tests to get and the nutrition and lifestyle changes that you need to make to address your hormone imbalances.
In relation to this particular topic, I wanted to thank you for your very informative summation of IUDs, and how they were designed to work. I’ve never used any form of hormonal birth control; I’ve always viewed it as a dishonest way of controlling my body (I mean, taking hormones to trick my reproductive system into functioning differently seemed sketchy from the outset), but people like you who are working so hard to inform women of all the details involved in these decisions can help us make truly empowered decisions for ourselves.
Having this information makes it that much easier for me to justify my own decisions; having this information makes women more likely to choose what’s best for their own health, and not just do what their doctor says, or their spouse, or their parents, or anyone else! So on a broader note, I just want to thank you for advocating for the natural functions of women’s bodies. Thank you for portraying our fertility as something normal and healthy. And thank you for doing it in such a patient, caring way! Your efforts are making such a positive impact on so many! Heck, even my husband is benefiting from information you’re sharing– I’ve convinced him to cut back on alcohol so that he won’t get so much estrogen building up in his system, haha.
P.S. I’m really looking forward to seeing your book! I have a feeling I’ll be getting more than one copy; this sort of stuff needs to be shared!
Thank you so much Lauren! Your lovely words perfectly encapsulate the reason I do this work so reading your comment made me so happy. Keep being a strong advocate for your health and tell you husband I’m proud of him too! 🙂 xoxo